Chapter: Medical Surgical Nursing: Assessment and Management of Problems Related to Male Reproductive Processes
Nursing Process: The Patient Undergoing Prostatectomy
NURSING
PROCESS: THE PATIENT UNDERGOING PROSTATECTOMY
Assessment
The nurse assesses how the underlying
disorder (BPH or prostate cancer) has affected the patient’s lifestyle. Has he
been reasonably active for his age? What is his presenting urinary problem
(de-scribed in his own words)? Has he experienced decreased force of urinary
flow, decreased ability to initiate voiding, urgency, fre-quency, nocturia,
dysuria, urinary retention, hematuria? Does the patient report associated
problems, such as back pain, flank pain, and lower abdominal or suprapubic
discomfort? If he reports such discomfort, possible causes include infection,
retention, and renal colic. Has he experienced erectile dysfunction or changes
in frequency or enjoyment of sexual activity?
The nurse obtains further information about the patient’s family history of cancer and heart or kidney disease, including hypertension.
Has he lost weight? Does he appear pale? Can he raise himself out of bed and
return to bed without assistance? Can he perform usual activities of daily
living? This information will help in determining how soon he will return to
normal activities after prostatectomy.
Diagnosis
Based
on the assessment data, the patient’s major nursing diag-noses may include the
following.
PREOPERATIVE NURSING DIAGNOSES
· Anxiety about surgery
and its outcome
· Acute pain related to
bladder distention
·
Deficient knowledge about factors related to the
disorder and the treatment protocol
POSTOPERATIVE NURSING DIAGNOSES
· Acute pain related to
the surgical incision, catheter place-ment, and bladder spasms
· Deficient knowledge
about postoperative care and man-agement
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based on the assessment data, the potential complications may include
the following:
· Hemorrhage and shock
· Infection
· Deep vein thrombosis
· Catheter obstruction
· Sexual dysfunction
Planning and Goals
The
major preoperative goals for the patient may include reduced anxiety and
learning about his prostate disorder and the peri-operative experience. The major
postoperative goals may include maintenance of fluid volume balance, relief of
pain and dis-comfort, ability to perform self-care activities, and absence of
complications.
Preoperative Nursing Interventions
REDUCING ANXIETY
The patient is frequently admitted to the
hospital on the morn-ing of surgery. Because contact with the patient may be
limited before surgery, the nurse must establish communication with the patient
to assess his understanding of the diagnosis and of the planned surgical
procedure. The nurse clarifies the nature of the surgery and expected
postoperative outcomes. In addition, the nurse familiarizes the patient with
the pre- and postoperative rou-tines and initiates measures to reduce anxiety.
Because the patient may be sensitive and embarrassed discussing problems
related to the genitalia and sexuality, the nurse provides privacy and
estab-lishes a trusting and professional relationship. Guilt feelings often
surface if the patient falsely assumes a cause-and-effect relation-ship between
sexual practices and his current problems. He is en-couraged to verbalize his
feelings and concerns.
RELIEVING DISCOMFORT
If discomfort is present before the day of
surgery, the patient is placed on bed rest, analgesic agents are administered,
and mea-sures to relieve anxiety are initiated. If the patient is hospitalized,
the nurse monitors the patient’s voiding patterns, watches for bladder
distention, and assists with catheterization if indicated. An indwelling
catheter is inserted if the patient has continuing urinary retention or if
laboratory test results indicate azotemia (accumulation of nitrogenous waste
products in the blood). The catheter can help to decompress the bladder
gradually over several days, especially if the patient is elderly and hypertensive
and has diminished renal function or an excessive amount of urinary re-tention
that has existed for many weeks. For a few days after the bladder begins
draining, the blood pressure may fluctuate and renal function may decline. If
the patient cannot tolerate a urinary catheter, he is prepared for a cystostomy
(see Chaps. 44 and 45).
PROVIDING INSTRUCTION
Before surgery, the nurse reviews with the
patient the anatomy of the affected parts and their function in relation to the
urinary and reproductive system, using diagrams and other teaching aids if
in-dicated. This is often done either during the preadmission test-ing visit or
in the urologist’s office. The nurse explains what will take place as the
patient is prepared for diagnostic tests and then for surgery (depending on the
kind of prostatectomy planned). The nurse describes the type of incision, which
varies with the type of surgical approach (directly over the bladder, low on
the abdomen, or in the perineal area; in the case of a transurethral procedure,
no incision will be made). The patient is informed about the type of urinary
drainage system that is expected, the type of anesthesia, and the recovery room
procedure. The amount of information given is based on the patient’s needs and
questions. Procedures expected during the immediate perioperative period are
explained, questions are answered, and support is provided. In addition, the
patient is instructed about postoperative use of medications for pain
management.
PREPARING THE PATIENT
When
the patient is scheduled for a prostatectomy. Elastic compression stockings are
applied before surgery and are partic-ularly important for prevention of deep
vein thrombosis if the pa-tient is placed in a lithotomy position during
surgery. An enema is usually administered at home the evening before surgery or
the morning of surgery to prevent postoperative straining, which can induce
bleeding.
Postoperative Nursing Interventions
MAINTAINING FLUID BALANCE
During
the postoperative period, the patient is at risk for imbal-anced fluid volume
because of the irrigation of the surgical site during and after surgery. With
irrigation of the urinary catheter to prevent its obstruction by blood clots,
fluid may be absorbed through the open surgical site and retained, increasing
the risk for excessive fluid retention, fluid imbalance, and water
intoxication. The urine output and the amount of fluid used for irrigation must
be closely monitored to determine if irrigation fluid is being retained and to
ensure an adequate urine output. The patient also is monitored for electrolyte
imbalances (ie, hyponatremia), rising blood pressure, confusion, and
respiratory distress. The risk for fluid and electrolyte imbalance is increased
in elderly patients with preexisting cardiovascular or respiratory disease.
These signs and symptoms are documented and reported to the surgeon.
RELIEVING PAIN
After a prostatectomy, the patient is
assisted to sit and dangle his legs over the side of the bed on the day of
surgery. The next morn-ing, he is assisted to ambulate. If pain occurs, the
cause and loca-tion are determined. It may be related to the incision or may be
the result of excoriation of the skin at the catheter site. It may be in the
flank area, indicating a kidney problem, or it may be due to bladder spasms.
Bladder irritability can initiate bleeding and result in clot formation,
leading to urinary retention.
Patients experiencing bladder spasms may note
an urgency to void, a feeling of pressure or fullness in the bladder, and
bleeding from the urethra around the catheter. Medications that relax the
smooth muscles can help to ease the spasms, which can be inter-mittent and
severe; these medications include flavoxate (Urispas) and oxybutynin
(Ditropan). Warm compresses to the pubis or sitz baths may also relieve the
spasms.
The
nurse monitors the drainage tubing and irrigates the sys-tem as prescribed to
relieve any obstruction that may cause dis-comfort. Usually, the catheter is
irrigated with 50 mL of irrigating fluid at a time. It is important to make
sure that the same amount is recovered in the drainage receptacle. Securing the
catheter drainage tubing to the leg or abdomen can help to decrease ten-sion on
the catheter and prevent bladder irritation. Discomfort may be caused by dressings
that are too snug, saturated with drainage, or improperly placed. Analgesic
agents are administered as prescribed.
When ambulatory, the patient is encouraged to
walk but not to sit for prolonged periods because this increases
intra-abdominal pressure and the possibility of discomfort and bleeding. Prune
juice and stool softeners are provided to ease bowel movements and to prevent
excessive straining. An enema, if prescribed, is ad-ministered with caution to
avoid rectal perforation.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
After
prostatectomy, the patient is monitored for major compli-cations such as
hemorrhage, infection, deep vein thrombosis, catheter obstruction, and sexual
dysfunction.
Hemorrhage
The
immediate dangers after a prostatectomy are bleeding and hemorrhagic shock.
This risk is increased with BPH because a hy-perplastic prostate gland is very
vascular. Bleeding may occur from the prostatic bed. Bleeding may also result
in the formation of clots, which then obstruct urine flow. The drainage
normally begins as reddish-pink and then clears to a light pink within 24 hours
after surgery. Bright-red bleeding with increased viscos-ity and numerous clots
usually indicates arterial bleeding. Venous blood appears darker and less
viscous. Arterial hemorrhage usu-ally requires surgical intervention (eg,
suturing of bleeders or transurethral coagulation of bleeding vessels), whereas
venous bleeding may be controlled by applying prescribed traction to the
catheter so that the balloon holding the catheter in place applies pressure to
the prostatic fossa. The surgeon applies traction by se-curely taping the
catheter to the patient’s thigh.
Nursing
management includes strategies to stop the bleeding and to prevent or reverse
hemorrhagic shock. If blood loss is ex-tensive, fluids and blood component
therapy may be adminis-tered.
Nursing
interventions include close monitoring of vital signs; administering
medications, intravenous fluids, and blood com-ponent therapy as prescribed;
maintaining an accurate record of intake and output; and careful monitoring of
drainage to ensure adequate urine flow and patency of the drainage system. The
pa-tient who experiences hemorrhage and his family are often anx-ious and
benefit from explanations and reassurance about the event and the procedures
that are performed.
Infection
After
perineal prostatectomy, the surgeon usually changes the dressing on the first
postoperative day. Further dressing changes may become the nurse’s
responsibility. Careful aseptic technique is used because the possibility for
infection is great. Dressings can be held in place by a double-tailed, T-binder
bandage or a padded athletic supporter. The tails cross over the incision to
give double thickness, and then each tail is drawn up on either side of the
scrotum to the waistline and fastened.
Rectal thermometers, rectal tubes, and enemas
are avoided be-cause of the risk for injury to and bleeding in the prostatic
fossa. After the perineal sutures are removed, the perineum is cleansed as indicated.
A heat lamp may be directed to the perineal area to promote healing. The
scrotum is protected with a towel while the heat lamp is in use. Sitz baths are
also used to promote healing.
Urinary
tract infections and epididymitis are possible com-plications after
prostatectomy. The patient is assessed for their occurrence; if they occur, the
nurse administers antibiotics as prescribed.
Because the risk for infection continues
after discharge from the hospital, the patient and family need to be instructed
to monitor for signs and symptoms of infection (fever, chills, sweats,
myalgias, dysuria, urinary frequency, and urgency). The patient and family are
instructed to contact the urologist if these symptoms occur.
Deep Vein Thrombosis
Because patients undergoing prostatectomy
have a high incidence of deep vein thrombosis (DVT) and pulmonary embolism, the
physician may prescribe prophylactic (preventive) low-dose hep-arin therapy.
The nurse assesses the patient frequently after surgery for manifestations of
DVT and applies elastic compression stockings to reduce the risk for DVT and
pulmonary embolism. The pa-tient who is receiving heparin must be closely
monitored for excessive bleeding.
Obstructed Catheter
After
a TUR, the catheter must drain well; an obstructed catheter produces distention
of the prostatic capsule and resultant hem-orrhage. Furosemide (Lasix) may be
prescribed to promote uri-nation and initiate postoperative diuresis, thereby
helping to keep the catheter patent.
The
nurse observes the lower abdomen to ensure that the catheter has not become
blocked. An overdistended bladder pre-sents a distinct, rounded swelling above
the pubis.
The drainage bag, dressings, and incisional
site are examined for bleeding. The color of the urine is noted and documented;
a change in color from pink to amber indicates reduced bleeding. Blood
pressure, pulse, and respirations are monitored and com-pared with baseline
preoperative vital signs to detect hypotension. The nurse also observes the
patient for restlessness, cold sweats, pallor, any drop in blood pressure, and
an increasing pulse rate.
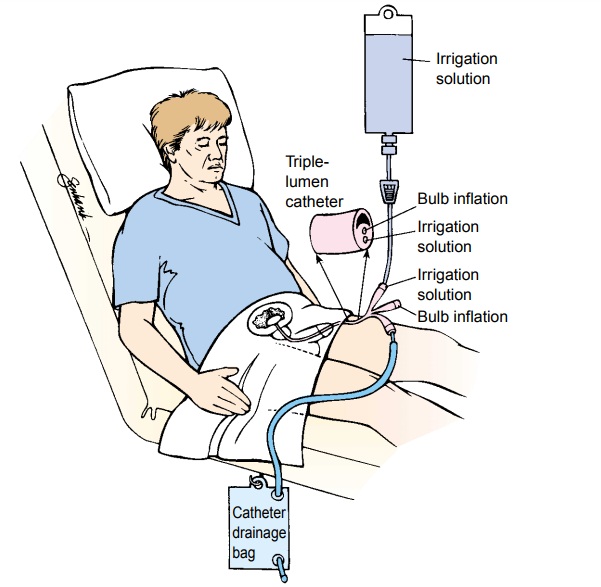
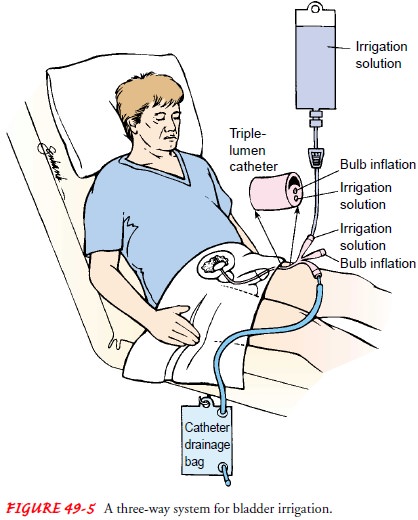
Drainage
of the bladder may be accomplished by gravity through a closed sterile drainage
system. A three-way drainage system is useful in irrigating the bladder and preventing
clot for-mation (Fig. 49-5). Continuous irrigation may be used with TUR. Some
urologists leave an indwelling catheter attached to a dependent drainage
system. Gentle irrigation of the catheter may be prescribed to remove any
obstructing clots.
If the patient complains of pain, the tubing
is examined. The drainage system is irrigated, if indicated and prescribed, to
clear any obstruction. Usually, the catheter is irrigated with 50 mL of
irrigating fluid at a time. The amount of fluid recovered in the drainage bag
must equal the amount of fluid injected. Over-distention of the bladder is
avoided because it can induce secondary hemorrhage by stretching the coagulated
blood vessels in the prostatic capsule.
The
nurse maintains an intake and output record, including the amount of fluid used
for irrigation.
The
drainage tube (not the catheter) is taped to the shaved inner thigh to prevent
traction on the bladder. If a cystostomy catheter is in place, it is taped to
the abdomen. The nurse explains the purpose of the catheter to the patient and
assures him that the urge to void results from the presence of the catheter and
from bladder spasms. He is cautioned not to pull on the catheter be-cause this
causes bleeding and subsequent catheter blockage, which leads to urinary
retention.
Complications With Catheter Removal
After
the catheter is removed (usually when the urine appears clear), urine may leak
around the wound for several days in pa-tients who have undergone perineal,
suprapubic, and retropubic surgery. The cystostomy tube may be removed before
or after the urethral catheter is removed. Some urinary incontinence may occur
after catheter removal, and the patient is informed that this is likely to
subside in time.
Sexual Dysfunction
Depending on the type of surgery, the patient
may experience sexual dysfunction related to erectile dysfunction, decreased
libido, and fatigue. These issues may become a concern of the pa-tient soon
after surgery or in the weeks to months during reha-bilitation. Erectile
dysfunction may occur following prostate surgery. Several options to restore
erectile function are discussed with the patient by the surgeon or urologist.
These options may include medications, surgically placed implants, or negative-pressure
devices. A decrease in libido may also occur following surgery and is usually
related to the impact of the surgery on the man’s body. Reassurance that the
usual level of libido will return following recuperation from surgery is often
helpful to the patient and his partner. The patient may also experience fatigue
during rehabilitation from surgery. This fatigue may also decrease his li-bido
and alter his enjoyment of usual activities.
Nursing interventions include assessing for
the presence of sexual dysfunction following surgery. Providing a private and
confidential environment to discuss issues of sexuality is impor-tant. The
emotional challenges of prostate surgery and its conse-quences need to be
carefully explored with the patient and his partner. Providing the opportunity
to discuss these issues can be very beneficial to the patient. For patients who
demonstrate sig-nificant problems adjusting to their sexual dysfunction, a
referral to a sex therapist may be indicated.
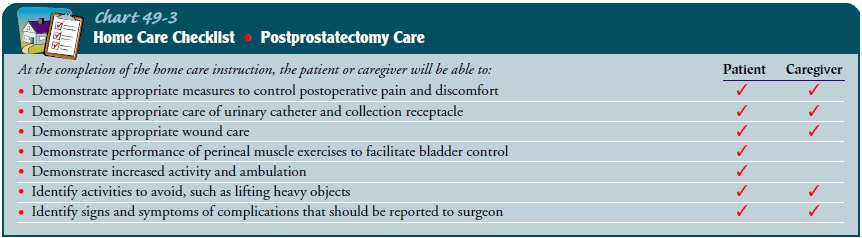
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
The patient undergoing prostatectomy may be
discharged within several days. The length of the hospital stay depends on the
type of prostatectomy performed. Patients undergoing a perineal prostatectomy
are hospitalized for 3 to 5 days. If a retropubic or suprapubic prostatectomy
is performed, the hospital stay is 5 to 7 days. The patient and family require
instructions about how to manage the drainage system, how to assess for
complications, and how to promote recovery. Verbal and written instructions are
provided about the need to maintain the drainage system and to monitor urinary
output, about wound care, and about strategies to prevent complications, such
as infection, bleeding, and throm-bosis. They are informed about signs and
symptoms that should be reported to the physician (eg, blood in urine,
decreased urine output, fever, change in wound drainage, calf tenderness).
As the patient recovers and drainage tubes
are removed, he may become discouraged and depressed because he cannot regain
bladder control immediately. Moreover, urinary frequency and burning may occur
after the catheter is removed. Teaching the following exercises may help the
patient regain urinary control:
· Tense the perineal
muscles by pressing the buttocks together; hold this position; relax. This
exercise can be performed 10 to 20 times each hour while sitting or standing.
· Try to interrupt the
urinary stream after starting to void; wait a few seconds and then continue to
void.
Perineal
exercises should continue until the patient gains full urinary control. The
patient is instructed to urinate as soon as he feels the first urge to do so.
It is important for the patient to know that regaining urinary control is a
gradual process; he may continue to “dribble” after being discharged from the
hos-pital, but the dribbling should gradually diminish (within up to 1 year).
Lining underwear with absorbent pads can help to min-imize embarrassing stains
on clothing. The urine may be cloudy for several weeks after surgery but should
clear as the prostate area heals.
While the prostatic fossa heals (6 to 8
weeks), the patient should avoid activities that produce Valsalva effects
(straining at stool, heavy lifting) because this increases venous pressure and
may produce hematuria. He should avoid long motor trips and strenuous exercise,
which increase the tendency to bleed. He should also know that spicy foods,
alcohol, and coffee may cause bladder discomfort. The patient is cautioned to
drink enough fluids to avoid dehydration, which increases the ten-dency for a
blood clot to form and obstruct the flow of urine. Signs of complications, such
as bleeding, passage of blood clots, a decrease in the urinary stream, urinary
retention, or urinary tract infection symptoms, should be reported to the
physician (Chart 49-3).
Continuing Care
Referral for home care may be indicated if
the patient is elderly or has other health problems, if the patient and family
cannot provide care in the home, or if the patient lives alone without
available supports. The home care nurse assesses the patient’s physical status
(cardiovascular and respiratory status, fluid and nutritional status, patency
of the urinary drainage system, wound and nutritional status) and provides
catheter and wound care, if indicated. The nurse reinforces previous teaching
and assesses the ability of the patient and family to manage required care. The
home care nurse encourages the patient to ambulate and to carry out perineal
exercises as prescribed. The patient may need to be reminded that return of
bladder control may take time.
The patient is reminded about the importance of participat-ing in routine health screening and other health promotion ac-tivities. If the prostatectomy was performed to treat prostate cancer, the patient and family are also instructed about the im-portance of follow-up and monitoring with the physician.
Evaluation
EXPECTED PREOPERATIVE PATIENT OUTCOMES
Expected preoperative patient outcomes may include:
·
Demonstrates reduced anxiety
·
States that pain and discomfort are decreased
·
Relates understanding of the surgical procedure and
post-operative course and practices perineal muscle exercises and other
techniques useful in facilitating bladder control
EXPECTED POSTOPERATIVE PATIENT OUTCOMES
Expected postoperative patient outcomes may include:
1) Relates relief of
discomfort
2) Exhibits fluid and
electrolyte balance
a)
Irrigation fluid and urinary output are within
parame-ters determined by surgeon.
b)
Experiences no signs or symptoms of fluid retention
3) Participates in
self-care measures
a)
Increases activity and ambulation daily
b)
Produces urine output within normal ranges and
con-sistent with intake
c)
Performs perineal exercises and interrupts urinary
stream to promote bladder control
d)
Avoids straining and lifting heavy objects
4) Is free of complications
a)
Maintains vital signs within normal limits
b)
Exhibits wound healing, without signs of
inflammation or hemorrhage
c)
Maintains acceptable level of urinary elimination
d)
Maintains optimal drainage of catheter and other
drainage tubes
e)
Reports understanding of changes in sexual function
Related Topics