Chapter: Essential Anesthesia From Science to Practice : Clinical management : General anesthesia
Induction, maintenance and emergence - General anesthesia
Induction, maintenance and emergence
Once the
preparations for general anesthesia are complete, the patient’s history and
physical examination are reviewed, the machine and equipment are set up and
tested, the patient is on the table, and the monitors are applied, we are ready
to send the patient on one of the strangest journeys of his life: general
anesthesia. We will administer drugs by injection and inhalation that will take
possession of the patient’s body. If we have used neuromuscular blocking
agents, ventilation will cease, and the patient will be unable to move. In
short, such an unconscious patient will have been reduced to a physiologic
organism without a will.
To
appreciate the enormity of this statement, consider the extreme of this
con-dition: once general anesthesia has been established for some cardiac
proce-dures, we might lower the patient’s temperature to the point where all
currently monitored variables cease to show evidence of life. There will be no
heartbeat, no electrocardiogram, no spontaneous breathing, and the
electroencephalogram will show no deflection. There will be no reflex, no
motion, and no reaction to any intervention. If, at this point, you were to
bring in an observer, unaware of what had been done, he might well pronounce
the patient dead. And yet, if we raise the temperature and initiate mechanical
ventilation, the patient’s cardiac and respiratory function will slowly resume
their own life and, once the temperature approaches normal and the effects of
drugs wear off, the patient will wake up. You might ask searching questions
about the patient’s state, his personality, his soul during this approach to
death. We cannot imagine a more profound responsibility than that of the
anesthesiologist taking a patient to such an extreme approxima-tion to death
while guarding his life.
In
routine general anesthesia we do not drive the system to the just described
extreme. Yet, a defenseless patient under general anesthesia will expect the
anes-thesiologist to stand in for him and his dignity and attend to him with
focused attention and great skill.
During
general anesthesia, we must provide the patient with sleep, amnesia, and
analgesia; we must monitor his vital signs and keep them within physiologic
limits, and we must make the surgeon’s task as easy as possible with the double
benefit of helping the surgeon so that she can do her best for the patient. But
before we start general anesthesia, an intravenous infusion (usually Ringer’s
lactate) is running, and we often give intravenously an anxiolytic with amnesic
power such as midazolam1 (1 to 2
mg for the average adult) and/or a narcotic, such as fentanyl (50 to 100 mcg
for the average adult). Some like to give the narcotic even though the patient
has no pain and even though the drug will not cause euphoria. Instead, it can
serve as a gentle background and preemptive analgesic for the operation and, by
weakening (but not eliminating) the sympathetic response, it can smooth out
swings of blood pressure and heart rate during intubation. We always keep in
mind the synergistic respiratory depression of a mixture of benzodiazepines and
opioids.
Pre-oxygenation
The
establishment of a patent airway is probably our most important safety concern.
Disaster overtakes the patient within a matter of minutes if he cannot breathe
for himself (because we paralyzed him), and we cannot ventilate his lungs
(because his airway is obstructed by soft tissue and because we cannot intubate
his trachea for any number of reasons). Then minutes, even seconds, count. If,
before inducing apnea, we replace the nitrogen in his lungs with oxygen, we can
gain 3 to 6 minutes (more with a large functional residual capacity (FRC))
before arterial hypoxemia occurs. Therefore, we routinely pre-oxygenate
patients before inducing anesthesia. This procedure is simple: we apply a face
mask and select a flow of oxygen high enough to prevent the patient from
inhaling his exhaled nitrogen. The latter is vented and, after about 3 minutes,
the patient’s FRC will contain very little nitrogen, much oxygen, and the usual
amount of water vapor and carbon dioxide.
Induction
We now
introduce hypnotic, analgesic, and anesthetic drugs into the body either by
intravenous injection or via the lungs (in the past intramuscularly or even
rectally). While inhalation anesthesia can be induced without the help of
intra-venous drugs, the most common approach is to inject a fast-acting drug
such as thiopental (3 to 5 mg/kg) or propofol (1 to 3 mg/kg). Within a couple
of minutes, these drugs will reach their peak effect, at which time intubation
of the trachea becomes feasible, usually with the help of muscle relaxants such
as succinyl-choline. Neither thiopental nor propofol offers relaxation of
muscles or analge-sia. Therefore, they are wonderful for gentle induction but
would be unlikely to provide adequate operating conditions for an
intra-abdominal procedure.
Instead
of intubating the trachea, we have the option of inserting a laryngeal mask
airway (LMA), which does not require the use of a muscle relaxant and is
par-ticularly welcome when the patient need not be intubated at all and is
breathing spontaneously throughout the operation (see Airway management
chapter).
Once we
have placed the endotracheal tube or LMA and have confirmed its proper location
by auscultation and end-tidal CO2, we can begin the adminis-tration
of inhalation, intravenous (TIVA, total intravenous anesthesia) or a
com-bination anesthetic. A number of halogenated drugs are available
(halothane, isoflurane, desflurane, sevoflurane), but we use only one at a
time. Each can be given together with 50–70% nitrous oxide in oxygen. Nitrous
oxide provides modest analgesic background without cardiovascular depression to
speak of. Surgical anesthesia (the patient will not respond to the incision)
can be obtained within a matter of minutes so that the induction of anesthesia
need not delay the incision.
Propofol
is the poster child agent for TIVA. Purported advantages of this tech-nique are
shortened wake-up and PACU times, and reduced risk of postoperative nausea and
vomiting. Rather than halogenated agents, patients for outpatient surgery might
receive a propofol infusion (for sedation and sleep) with nitrous oxide to
provide a modicum of analgesia and ensure amnesia, supplemented with small
amounts of analgesics.
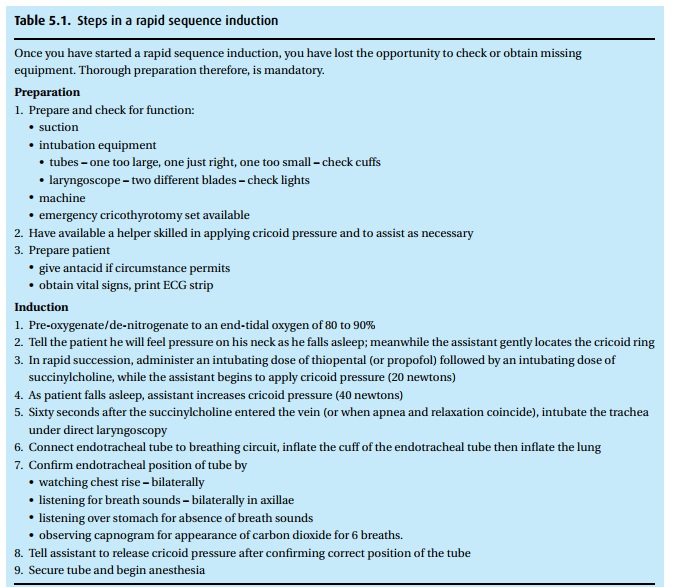
The rapid sequence induction
Patients
who need general anesthesia, even though they have a full stomach (hav-ing
recently eaten or having a condition that interferes with gastric emptying such
as trauma or pregnancy), require a special technique, the so-called rapid sequence
induction (Table 5.1). With a full stomach,
the specter of regurgitation and aspir-ation arises. The technique calls for a
thorough denitrogenation, followed by the administration of thiopental and
succinylcholine in rapid succession while we maintain pressure on the cricoid
ring (the so-called Sellick maneuver2).
Remem-ber, the cricoid is the only ring of the trachea that does not have a
membrane posteriorly and, instead, is cartilaginous throughout its
circumference. So, push-ing on it compresses the esophagus. You can feel the
cricoid ring just under the larynx. Only once we have confirmed the proper
position of the endotracheal tube and inflated the cuff can we stop the Sellick
maneuver.
Positioning
For many
operations, the patient can lie on his back. Others require positions that may
take an hour or more to be accomplished (for example, neurosurgical
operations). We need to understand what position favors access for the surgeon
and what positions present dangers for the patient (interference with
ventila-tion, compression of nerves, extreme flexion or extension of joints).
Thus, the positioning is often a joint surgical/anesthesia task during which a
lot of foam padding finds application between patient and hard surfaces. The
most common post-operative nerve palsy affects the ulnar nerve (funny bone),
which is exposed to pressure, being superficial and running through the ulnar
groove at the elbow (between the medial epicondyle and the olecranon).
Depth of anesthesia and monitoring
Once the
patient is positioned, we must keep the anesthetic level so that the patient
will neither feel pain nor remember the operation. Yet this “anesthetic depth”
must be balanced against the hemodynamic consequences (hypotension) of excess
anesthetic, as well as the potential for delayed wake-up. If the patient is not
paralyzed, there will be little doubt that he will move and let us know if he
feels pain. We need to gauge the depth of anesthesia clinically and with the
help of instruments. The clinical assessment includes monitoring heart rate and
blood pressure, which should be neither high from sympathetic response to
noxious stimulation, nor low from overdose with anesthetics. In recent years
processed EEG signals have become available that claim to help gauge the depth
of anesthesia by generating a score linked to EEG activity, which becomes
depressed as anesthesia deepens. In addition to these signals we keep track of
the intravenous drugs the patient has had, of their effects and duration, and
of the concentration of expired anesthetics, which reflect blood and finally
brain levels. Thus the conduct of general anesthesia calls for continual
attention to a number of parameters and variables.
At the
same time, we monitor pulse oximetry, blood pressure, heart rate, ECG, tidal
volume, respiratory rate and peak inspiratory pressure, inspired oxygen, the
concentration of respired gases and vapors, and the capnogram. Should blood
loss, deep anesthesia, surgical activity (for example compressing the vena
cava), an embolism (for example, air aspirated in an open vein), or a process
originating in the patient (such as anaphylaxis or coronary insufficiency)
cause a problem, we should be able to discover the effects as early as possible
so that we can take corrective actions. We also assess the degree of muscle
relaxation with the help of a nerve stimulator (twitch monitor) and by watching
the operation and gauging muscle tone, which might impede the surgeon’s work.
Thus, we cannot be satisfied with watching the monitors; we need to keep an eye
on the patient, his face, his position, and the surgeon’s work.
A
tedious aspect of our work is the obligation to keep a record of all these
events and of our activities, such as the administration of drugs and fluids,
adjustment of ventilator settings, and even of surgical events (“aorta clamped
at 9:24 am!”). Automated record keeping systems are becoming increasingly
sophisticated.
Emergence
Well
before the surgeon puts in the last stitch, we begin preparation for having the
patient wake up. This might call for the reversal of a non-depolarizing
neuromuscular blocking drug and the scaling back of inspired anesthetic
con-centrations. Furthermore, our goal is to have the patient awaken quickly
and without pain; therefore, we titrate opioids or our regional anesthetic to
anticipate the pain level without unacceptable respiratory depression, while
also consider-ing the risk for postoperative nausea and vomiting. It is a fine
art to gauge the surgical process and the patient’s requirements so that the
patient opens his eyes when the dressing goes on. “Hello,” we say, and, after
confirming the patient is strong, able to protect his airway (gag reflex),
breathing and following commands, we suction his airway and say, “All done! Let
me take out that tube,” when we pull the endotracheal tube or the LMA. While
the patient is not likely to remember such words, they provide a fitting ending
to a perfect anesthetic!
We then
accompany the patient to the Post-Anesthesia Care Unit (PACU) where we go
through a formal process of turning the care of the patient over to a
spe-cialized PACU nurse, unless the patient is fit for early discharge home or
needs to be admitted to the Intensive Care Unit.
Related Topics