Chapter: Basic Radiology : Musculoskeletal Imaging
Exercise: Systemic Disease
EXERCISE 6-3.
SYSTEMIC DISEASE
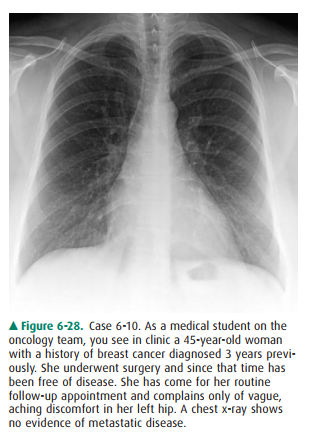
6-10. For Case 6-10
(Figure 6-28), which of the following studies would be least useful today?
A.
Chest CT
B.
Left hip x-ray
C.
Bone scan
D.
Skeletal survey
E.
Mammography
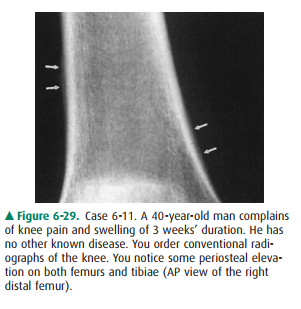
6-11. For Case 6-11
(Figure 6-29), what is the next study you should order?
A.
Bone scan
B.
MRI of the knee
C.
Hand films
D.
Chest radiograph
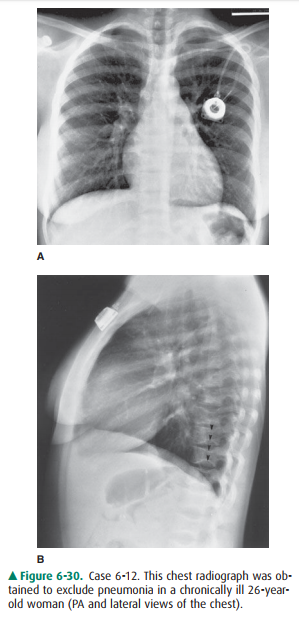
6-12. For Case 6-12
(Figure 6-30), there is no evidence of pneumonia, but there are several
abnormalities that are clues to the nature of this patient’s chronic illness.
Which finding is such a clue?
A.
The presence of a central venous line
B.
Enlargement of the pulmonary artery segment of the mediastinum
C.
Depression in the endplates of numerous vertebrae
D.
Asymmetry of the breast shadows
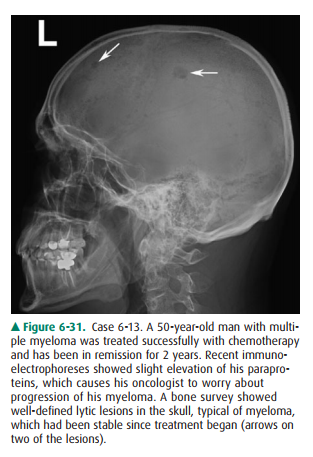
6-13. For Case 6-13
(Figure 6-31), which of the following imaging tests is most likely to help
determine if this patient has progressive myeloma?
A.
PET-CT
B.
Bone Scan
C.
Chest x-ray
D.
CT of the spine
Radiologic Findings
6-10. D is the correct
answer to Question 6-10.
6-11. A thin rim of
calcium added to the bony contour of both sides of the right femoral metaphysis
(Figure 6-29, arrows) is due to periosteal elevation. Similar findings were
present on the left femur and both tib-iae (D is the correct answer to Question
6-11).
6-12. Many vertebral
bodies, as best appreciated in the lat-eral view, are shaped like the letter H
(arrowheads), with central depressions in the superior and inferior end plates.
(Figure 6-30) (C is the correct answer to Question 6-12).
6-13. A is the correct
answer to Question 6-13.
Discussion
Case 6-10: Option E, mammography,
is a reasonable screen-ing examination. This would be a good test to order for
this patient even without new symptoms. Indeed, mammogra-phy should be obtained
in any woman of 45 years every year for screening purposes, irrespective of her
history. Bone scans are also often ordered as screens for metastatic diseasein
asymptomatic breast cancer patients, particularly for the first 2 to 3 years
after diagnosis. Because this patient is com-plaining of skeletal pain, both a
bone scan (Figure 6-32 A) and conventional radiographs of the affected area
(Figure 6-32 B) are indicated. A chest CT can be helpful to find small
pulmonary metastases that may not be apparent on a conventional chest radiograph.
Whether to order it for this woman may depend in part on the preferences of the
attend-ing oncologist and on risk factors such as the size of the orig-inal
tumor and nodal status at the time of diagnosis. Option D, a skeletal survey,
is inappropriate. Bone surveys are gener-ally utilized in breast cancer only
for follow-up of patients with widespread osseous metastatic disease.
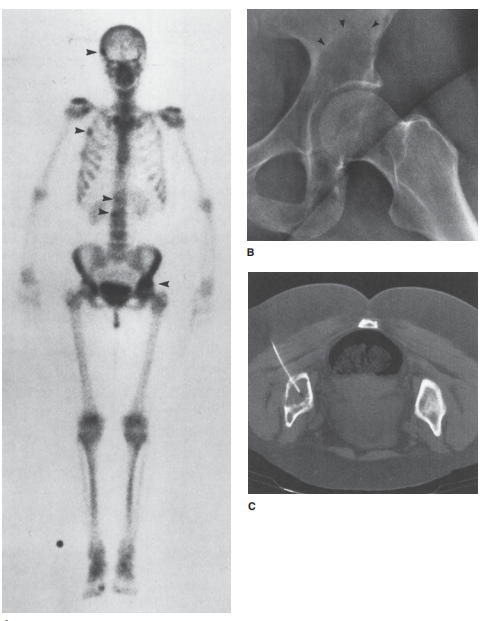
In this patient’s case, a bone
scan revealed multiple areas of abnormally increased accumulation of
radionuclide, includ-ing the left acetabulum (Figure 6-32 A,B). The
multiplicity of lesions, together with the history of breast cancer (which
often metastasizes to bone and may do so after a disease-free inter-val of many
years), is very suggestive of metastatic disease. Some oncologists would choose
to treat the patient for pre-sumed metastatic disease on the basis of the bone
scan, his-tory, and current symptoms. Others would prefer a biopsy before
proceeding to further treatment. This patient under-went a CT-guided needle aspiration
of the acetabular lesion, which revealed metastatic tumor (Figure 6-32 C). To
evaluate for possible impending pathologic fracture (Figure 6-33), most
oncologists would also request conventional radi-ographs of areas demonstrating
increased activity on the bone scan, particularly those in weight-bearing
bones.

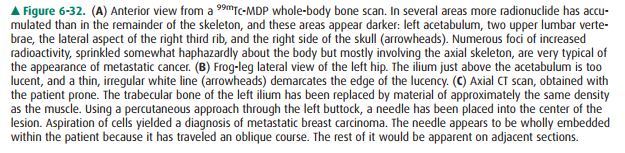
Case 6-11: Periosteal elevation
is a nonspecific finding that occurs with local disorders such as fracture,
bone tu-mors, and osteomyelitis and also with systemic or multifocal disorders
such as bone infarction (Figure 6-34), venous sta-sis, and secondary
hypertrophic osteoarthropathy. Because this finding is bilateral, it is more
likely due to a systemic or multifocal disorder than to a local one.
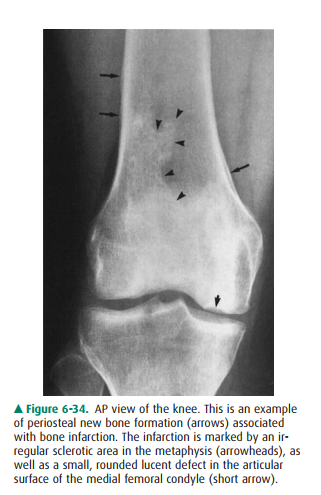
Of all systemic disorders that
may be associated with pe-riosteal new bone formation, secondary hypertrophic
os-teoarthropathy is the most important to exclude. At one time it was called
hypertrophic pulmonary osteoarthropathy be-cause it is usually caused by
pulmonary disease. The designa-tion secondary hypertrophic osteoarthropathy
reflects current understanding that this disorder may also be due to
nonpulmonary diseases such as inflammatory bowel disease or congenital cardiac
anomalies. Nonetheless, pulmonary disease, specifically lung cancer, remains
the most common cause. This patient, in fact, had lung cancer (Figure 6-35).
A bone scan could be useful if
you did not notice the pe-riosteal new bone or were not sure of its presence.
Hand films could demonstrate clubbing, which may be seen with some of the same
disorders that cause hypertrophic osteoarthropathy, but simple physical
inspection of the patient’s hands would accomplish the same thing. MRI of the
knees will not be helpful in this case.
Case 6-12: This patient (see
Figure 6-30) has sickle cell disease. The peculiar shape of multiple vertebral
bodies is very characteristic of sickle cell anemia, though it may
occa-sionally be seen in other diseases affecting the marrow cavity, particularly
Gaucher’s disease. It may be caused by infarction of bone beneath the
endplates, with remodeling of the cortex to produce the H-shape.
When red cells sickle, they clump
together and may block blood vessels. In bone this leads to avascular necrosis,
which may be widespread, involving many bones simultaneously. The mottled
appearance of this patient’s humeral heads is due to avascular necrosis and is
a common finding in patients with sickle cell anemia.
Though they were not included
among the possible answers to the question, there are other findings on this
examination that are clues to the diagnosis. The gas-filled splenic flexure of
the colon occupies too much of the left upper quadrant on the frontal view.
There is no room for a spleen of normal size. In sickle cell patients, the
spleen is often infarcted so that by any time they reach adulthood, it has
shrunk to a small fraction of normal size. People with sickle cell disease are
prone to early de-velopment of calcium bilirubinate gallstones (cholelithiasis).
Modest enlargement of the
pulmonary artery, as seen in this patient, is so common in young women that it
is consid-ered normal in that population. The central line may be seen in many
patients with a variety of disorders requiring chronic intravenous therapy.
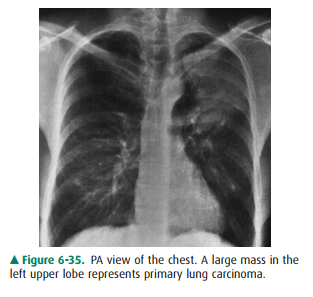
Case 6-13: Multiple myeloma is a
disease that can never really be considered cured. The goals of therapy are
control ofsymptoms and, if possible, induction of remission. Remis-sion may
last months or even years, and during remission the patient is monitored for
any signs that the disease has re-turned and is progressing. In this patient’s
case, the oncolo-gists are looking for any imaging-based evidence of disease
progression to back up a fairly weak clinical indicator.
A challenge is that the patient
is already known to have lytic bone disease. Even though the myeloma has been
in re-mission, the lytic lesions will not have gone away. Therefore, imaging
studies that rely primarily on anatomy will only be helpful if they
unequivocally show evidence of new lytic le-sions. The bone survey has already
been asserted to be un-changed, so no other conventional radiographs are likely
to be helpful, either. Therefore, a chest x-ray will not be a good choice. CT
scans are also anatomically based tests and can be expected to show lytic
lesions without necessarily helping to determine if the lesions are old and
quiescent or if they are actively growing.
What is needed is a test that
will assess the metabolic ac-tivity of this patient’s multiple myeloma,
preferably with some associated anatomic information. MRI may be helpful in
such situations. It is a good anatomic test, and if contrast is given, it also
demonstrates areas of hyperemia. MRI, how-ever, was not one of the answer
choices. Bone scans are meta-bolic tests, but myeloma is a notorious source of
false negative bone scans.
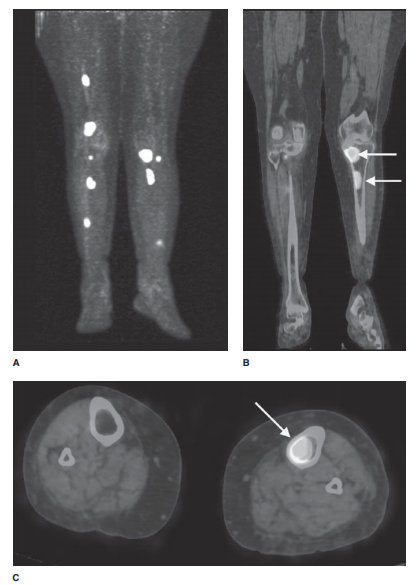
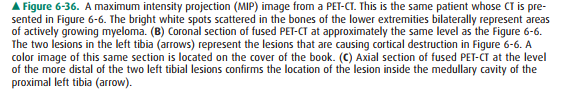
PET-CT may be quite useful for
differentiating quies-cent from metabolically active, growing lesions of
myeloma (Figure 6-36).
Related Topics