Chapter: Basic Radiology : Musculoskeletal Imaging
Musculoskeletal Imaging: Techniques
TECHNIQUES
Conventional Radiography
Conventional radiographs are the
most frequently obtained imaging studies. They are chiefly useful for
evaluation of the bones, but useful information about the adjacent soft tissues
may also be obtained. Gas in the soft tissues may be a clue to an open wound,
ulcer, or infection with a gas-producing or-ganism. Calcifications in the soft
tissues can indicate a tumor, myositis ossificans, or systemic disorders such
as scleroderma or hyperparathyroidism.
To get the most information
possible from conventional radiographs, you should carefully choose the study
to be or-dered. At most hospitals and clinics, standardized sets of views have
been developed that are routinely obtained to-gether for evaluation of specific
body areas in certain clinical settings. It is useful to know what will
routinely be obtained when a certain set of films is ordered. Radiographs of
the ankle, for example, usually include a straight frontal view of the ankle, a
frontal view obtained with approximately 15 degrees internal rotation of the
ankle (the mortise view), and a lateral view. There will be some variation
among institutions, however. At a minimum, two views at right angles to one
an-other should be obtained when a fracture or dislocation is suspected,
because such injuries are notorious for being very subtle or even invisible in
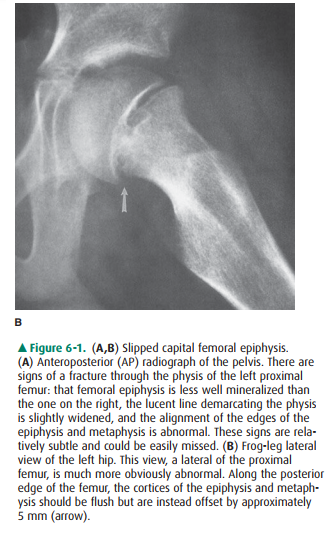
one projection, even when they are glaringly obvious in another view (Figure
6-1). Radiographs should be focused on the anatomic area being evaluated, free
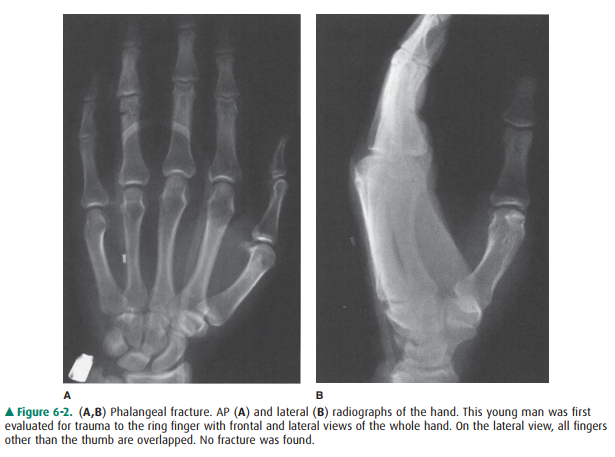
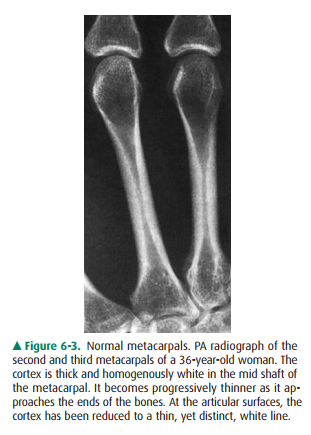
of overlapping, extraneous anatomy (Figure 6-2). If the kneeis the site of
trouble, do not order views of the entire tibia and fibula; you will be
disappointed with the visualization of the knee. This principle must be
abandoned more or less in young children and mentally impaired individuals who
may not be able to localize their symptoms well, and also in trauma victims
with so many injuries that the relatively minor ones may be overlooked.
In addition, when the radiographs
will be studied by a consulting radiologist, it is helpful to provide a
succinct yet accurate history pinpointing your clinical concerns. Simply
indicating the site of injury will improve the likelihood that a subtle
fracture will be discovered.
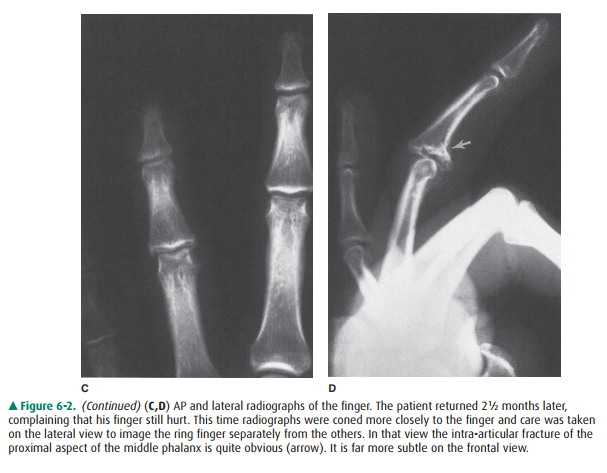
A conventional radiograph of a
normal bone will show a smooth, homogenous cortex surrounding the medullary
space. The cortex will be thicker along the shaft (diaphysis) of long bones and
thinner in small, irregular bones such as the carpal and tarsal bones and at
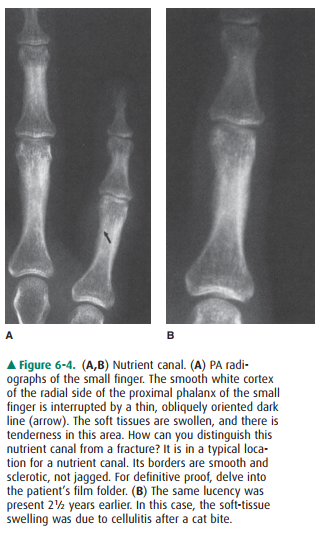
the ends of long bones (Figure 6-3). Exceptions are the normal roughening of
the cortex at tendon and ligament insertion sites and the normal interrup-tion
of the cortex at the site of the nutrient arteries. Naturally these occur at
predictable places that differ from bone to bone. Within the medullary space of
normal bone are trabec-ulae. These are visible in radiographs as thin, crisp
white lines that are arranged not randomly but in predictable patterns that
enhance the stress-bearing capability of the bone.
When questions arise concerning
whether a particular appearance is normal or abnormal, several solutions are
possible. Two books, Keats’s Normal
Variants and Kohler’s Borderlands,
are very useful in helping to distinguish the nor-mal from the abnormal (see
suggested reading). Correlation with the results of the history and physical
examination may also be helpful. Finally, comparison with the patient’s prior
radiographs or with a radiograph of the opposite extremity may also help (Figure
6-4). Comparison views of the oppo-site extremity are especially helpful in
children, in whom the open physes and accessory centers of ossification may
vary considerably from individual to individual but tend to vary less from side
to side than among different people.
Mammographic
Techniques
Any soft-tissue area that can be
pulled away from the skeleton and placed between the compression paddle and
detector may be imaged with mammographic technique. In extremity imag-ing,
mammographic technique is occasionally used to search for small calcifications
or foreign bodies in the soft tissues.
Fluoroscopy
Fluoroscopy plays an important
role in evaluation of joint mo-tion. It is often used by orthopedic surgeons to
monitor place-ment of hardware. It may be of assistance in positioning patients
for unusual or difficult conventional radiographic views.
Computed Tomography
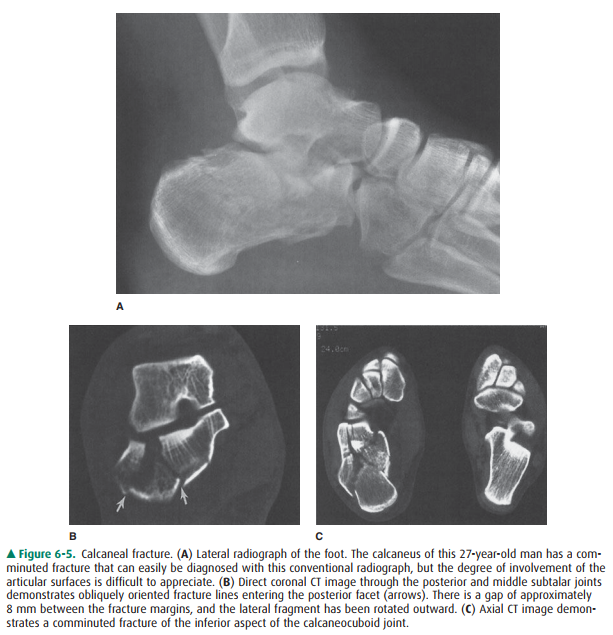
Tomography (either conventional
complex-motion tomog-raphy or computed tomography [CT]) has two major uses in
skeletal imaging. The first is evaluation of fracture frag-ment position. CT
provides excellent delineation of fractures purposes, as they can often be
understood by less experienced individuals. They do not, however, contain
information be-yond that available in tomographic images.
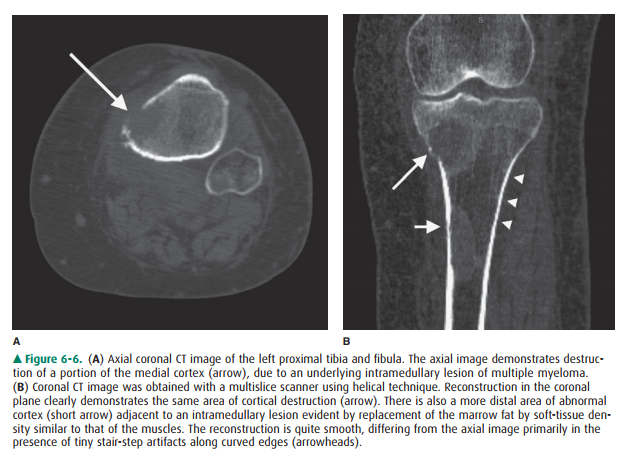
The second major use of CT is in
evaluation of bone tu-mors or tumor-like diseases. For this purpose, magnetic
reso-nance (MR) imaging is the principal competing technique. CT is more
sensitive than MRI in demonstrating small amounts of calcium and can show early
periosteal new bone formation or small amounts of matrix calcification before
they may be seen with conventional radiography. This finding can be helpful in
narrowing the differential diagnosis of a tumor. MRI can easily obtain images
in sagittal and coronal planes, which was once an advantage this technique had
over CT. Multislice CT scan-ners have negated this advantage (Figure 6-6).
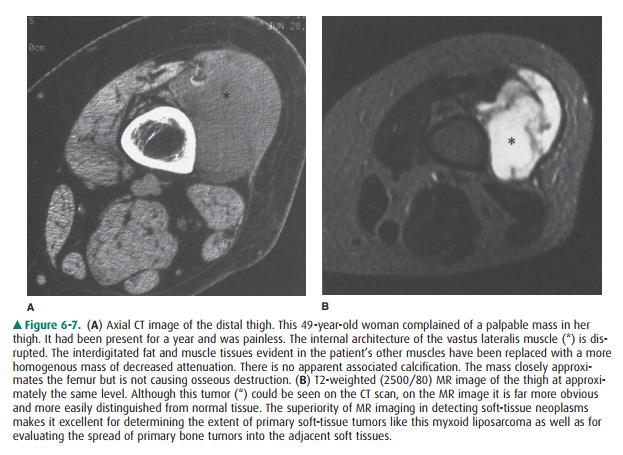
Before MRI was developed, CT was also used widely for determining the extent of
soft-tissue tumors, including osseous tumors that have spread into the soft
tissues. MRI, however, is now more often used for staging. Its superior
contrast resolution greatly eases the task of determining tumor extent within
bone marrow and muscle or other soft tissues (Figure 6-7).
Magnetic Resonance Imaging
The exquisite contrast of MRI
makes it ideal for evaluation of soft tissues. Its most frequent use in
skeletal imaging, there-fore, is for diagnosis of injuries to muscles, tendons,
or liga-ments about joints. This superb contrast resolution also makes it very
useful for evaluating disorders of the bone mar-row including neoplasm, marrow-packing
diseases such asGaucher’s disease, osteomyelitis, fractures that are occult on
conventional radiographs, and avascular necrosis. Unfortu-nately, although MRI
is very sensitive to these abnormalities, it is also very nonspecific. Many
diseases of marrow cause similar signal alteration. One must then narrow the
differen-tial diagnosis based on the distribution of the abnormalities
together, the radiographic appearance, and the clinical his-tory.
Diffusion-weighted MR imaging may be used to identify areas of an organ that
have recently been damaged or injured. Diffusion-weighted MR imaging of the
vertebral body may differentiate benign from malignant fracture, although its
usefulness is still controversial.
Nuclear Medicine
Several nuclear medicine studies
are used for skeletal dis-ease. The two most common are the technetium bone
scan and fused positron emission tomography and computed to-mography (PET-CT).
One of several phosphate compounds of technetium-99m is selected for use in
bone scan. Methyl-ene diphosphonate (MDP) is used most frequently. If there is
a specific anatomic area of interest, images may be ac-quired over that area at
the time the radionuclide is injected, as well as 3 to 4 hours later. The
immediate images reflect the amount of blood flow to the area; the delayed
images reflect the amount of bone remodeling occurring there.
Bone scintigraphy is a sensitive
but not very specific tech-nique. Most osseous abnormalities of clinical
significance will cause an increase in radionuclide accumulation. Exceptions
are destructive lesions that incite little reparative reaction in the host bone
or that destroy bone so quickly that it cannot remodel.
Because of their sensitivity and
because they provide physiologic rather than anatomic information, bone scans
can be used to find abnormalities before they are detectable by conventional
radiography. In particular, they are often used for screening for bone
metastases in patients with known malignancy. Both multiple myeloma in adults
and Langerhans cell histiocytosis in children, however, are notori-ous for
causing no increased accumulation on bone scans. Therefore, in these diseases
conventional radiographs or skeletal surveys are better than bone scans for
screening for osseous involvement. MR imaging is sometimes also used for
screening for myeloma or metastatic disease.
Fused positron emission
tomography–computed tomogra-phy (PET/CT) combines in a single gantry system
both PET scanner and CT scanner, so that images acquired from both techniques
can be taken sequentially in the same session and combined into a single
superimposed image. Thus, functional imaging obtained by PET, which depicts the
spatial distribution of metabolic or biochemical activity in the body, can be
more precisely aligned or correlated with anatomic imaging obtained by CT
scanning. Other imaging studies may also be fused to combine metabolic
information of a nuclear study with anatomic information. For example, a SPECT
bone scan may be combined with CT or a PET scan may be combined with MRI.
Biopsy
When tumor or infection is
suspected, it is often useful to ob-tain a tissue sample for cytologic or
histologic analysis or for culture. This may be accomplished by means of an
“open” procedure in the operating room or a percutaneous needle puncture of the
lesion to obtain a cellular aspirate or slender core of tissue. Needle biopsies
of palpable lesions do not nec-essarily need radiologic intervention. When the
lesion is not palpable, however, biopsy may be accomplished under
fluo-roscopic, CT, ultrasound, or MRI guidance.
When skeletal lesions should be
biopsied and by whom are important questions that can have a tremendous impact
on the patient’s outcome. For example, sarcomas have been reported to grow
along the surgical or needle tracks after diagnostic biopsies. Therefore, when
planning biopsies of suspected mus-culoskeletal sarcomas, care must be taken to
approach the le-sion through a track that can be resected en bloc with the
tumor at the time of ultimate excision. These biopsies should always be carried
out in close consultation with the surgeon who will be performing the
definitive surgery.
When systemic disease such as
metastatic carcinoma is the primary consideration, percutaneous needle biopsy
is the most efficacious means of making a diagnosis if the lesion is amenable
to this procedure. In this setting, the yield of needle biopsy is very good
(90% or more of such biopsies yield a positive diagnosis when tumor is truly
present) and a nega-tive result is less likely to lead to open biopsy than it
would in some suspected primary tumors. Nonetheless, biopsy should still be
performed in consultation with the oncologist or other physician giving overall
care.
Related Topics