Chapter: Medicine Study Notes : Musculo-Skeletal
Back Pain
Back Pain
Sources of Pain
·
Local: processes compressing or
irritating nerve endings, e.g. fractures or tears. If it does not vary with
change in position then ?spinal tumour or infection
·
Pain referred to spine: arises
from abdominal or pelvic viscera. Often
unaffected by position of spine
·
Pain of spinal origin: Upper
lumbar refers to groin or anterior thighs. Lower lumbar refers to buttocks,
posterior thighs or calves/feet
·
Radicular back pain: sharp and
radiates from spine to leg in territory of nerve root. Coughing, sneezing or
voluntary contraction of abdominal muscles often elicits radiating pain. Increase
pain in postures which stretch the nerve root (e.g. sciatic nerve – L5 & S1
- when sitting as it passes posterior to hip, but not femoral nerve – L2 – L3
as it passes in front of the hip)
·
Pain associated with muscle
spasm: accompanied by abnormal posture, taut para-spinal muscles and dull pain
·
Very hard to differentiate lower
back pain ® cheat and call it lumbar spine dysfunction!
Classification
·
Pathological (5%): infection,
inflammation, metabolic bone disease, neoplasm
·
Referred (5%): Abdominal or
pelvic organs
·
Mechanical (95%):
o Muscle/ligament injury
o Intervertebral disc injury
o Spondylolysis and spondylolisthesis
Age
·
Children: congenital or
developmental disorders, infection, primary tumours (ie don‟t ignore back pain
in children)
·
Younger adults: disc disease,
spondylolisthesis, acute fractures
o Older adults: spinal stenosis, metastatic disease, osteopenic
compression
Injuries
·
Hyperflexion ® wedge
fracture around T12 – L 2
·
Shearing ® anterior
or posterior displacement, intervertebral ligaments torn
·
Hyperextension: tears
longitudinal ligaments, widens anterior disk space
·
Axial compression: squeezes T4 –
L5 ® disc squeezes out and disrupts longitudinal ligaments
·
Spondylolysis: defect/fatigue
fracture in the pars interarticularis. Most common cause of low back pain in
children and adolescents. Defect in the neck of the „Scottie dog‟ on oblique
x-rays
Mechanical Back Pain
·
No obvious pathology – following
trauma or progressive onset. But major
cause of people off-work etc
·
Spinal movement is complex Ăž there
are many components that could cause pain
·
Not related to old age: most
common in 25 – 60 year olds
·
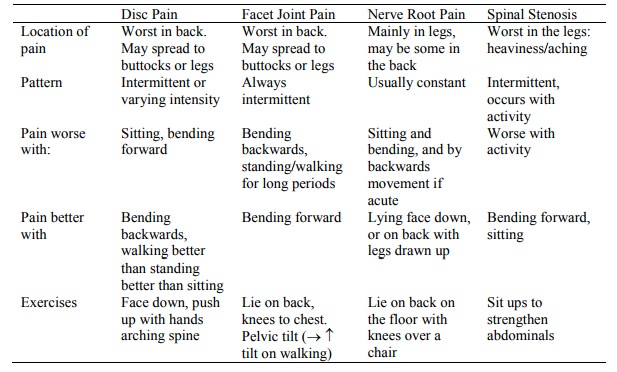
Patterns:
·
Lumbar Spondylosis:
o Degeneration of joints and of intervertebral discs
o Gel of nucleus pulposis shrinks and looses compliance causing
circumferential bulging of annulus fibrosis.
o Osteophytes may form
o Most common sites are L5/S1 and L4/L5
o Facet joint syndrome – secondary osteoarthritis of the facet
joints. Pain worse bending backwards
o Presentation: midline pain radiating to groin or buttock, worse towards
the end of the day, aggravated by coughing or sneezing. Straight leg raising is
normal
o Treatment: analgesics, physio, spinal fusion
·
Acute lumbar disc prolapse:
o Nucleus pulposis extrudes into a fissure in the annulus and bulges
beneath the posterior longitudinal ligament:
§ Pressure on ligament ® back ache
§ Pressure on dural envelope of the nerve root ® pain
referred to lower limbs (sciatica)
§ Compression of nerve root ® paraesthesia and muscle weakness
o Posture: stand forwards and sideways tilt
o Sudden onset lasting for hours/days.
Local tenderness and loss of spinal mobility
o Differential:
§ Inflammation (eg due to Ankylosing Spondylitis or Tb)
§ Vertebral tumours ® constant pain
§ Nerve tumours cause sciatic but constant pain
o X-ray to exclude bone disease.
CT/MRI best for localising the lesion
o Treatment:
§ Rest: most resolve spontaneously
§ Reduction: continuous bed rest and pelvic traction for 2 weeks
§ Removal: if cauda equina compression, persistent pain after 2 weeks or
neurological deterioration
§ Rehabilitation: isometric exercises and advice on bending/lifting
·
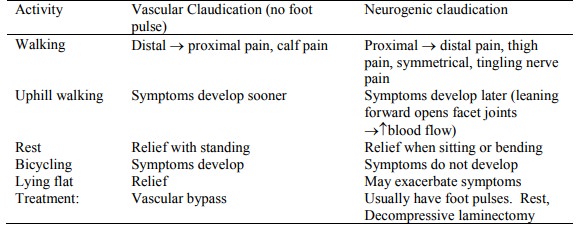
Spinal and root canal stenosis:
o Due to progressive loss of disc height, OA of facet joints, posterior
osteophytes
o Rarely ® neurogenic claudication (nerve root ischaemia) when walking. Due to ¯ blood
flow to the cauda equina (whose metabolic needs  on
walking)
o Differential of vascular and neurogenic claudication:
Spondylolisthesis:
o Anterior or posterior displacement of a vertebrae with or without preceding injury (usually L5 slides forward on S1)
o Can be congenital (eg defect of articular processes) or acquired (trauma, OA of facet joints, pathological, fracture of the neural arch, elongation of the pars interarticularis)
o Requires bilateral interarticular defect ®
instability
o X-ray (AP and lateral) if:
§ < 20 years or > 50 years
§ Suspicious pain
§ Worse at night and in morning (inflammation, infection, tumour)
§ Neurological signs (® CT/MRI)
o Management:
§ Conservative: lumbosacral support, exercises to build extensor and abdominal
muscles
§ Surgery: Nerve release and spinal fusion
·
Other non-mechanical back-pain:
o Sway Back: pregnancy: altered spinal posture and ligamentous
laxity. Conservative treatment
o Osteoporotic: painless or agonising localised pain that radiates around ribs and abdomen. Caution
o with spine physio: mechanical lever arm forces on vertebrae are very
strong ® easy damage
o Psychogenic pain is a contributing factor in some. Look for signs of secondary gain
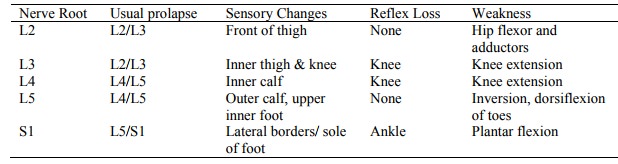
Localisation of Lumbar Root Nerve Entrapment
Red Flags
·
Continuous or progressive pain
which doesn‟t change with movement
·
Fever (e.g. infection)
·
Bowel/bladder involvement (sacral
roots)
·
Also:
o Young (< 20) or old (> 55)
o Violent trauma: MVA or fall from a height
o Bilateral or alternating sciatica
o Weak legs
o Weight loss
o ÂESR
o On oral steroids
o IV Drug use
o Pain with movement in all directions
o Localised bony tenderness
o Past history of neoplasia
o CNS deficit at more than one root level or bilateral
·
If no red flags then
investigations not indicated unless symptoms persist beyond 4 – 6 weeks
Yellow Flags
·
= Barriers to recovery
·
Problems at home or work
Management of Back Pain
·
Conservative:
o 80 – 90% of back pain resolves in 4 – 6 weeks
o Firm bed (eg a board underneath)
o No slouching, education on how not to stress back
o Analgesia (® break cycle of muscle spasm)
o No bed rest, early return to work
o Warmth, analgesics
o Promote self care and responsibility ® ¯dependence
o Stay active. Eg swimming. But may need to modify normal activities. Lift carefully, wear low healed shoes, chair which helps good posture, pillow between knees at night, walking, cycling, swimming
o Exercises only help with symptoms – don‟t affect recovery time
o Physio – but not while acutely sore
o Manipulation may help in the first month
o Advice on prevention
o Check-ups at 1, 4 and 6 weeks (ACC guidelines)
o If not improved after 2 weeks, consider X-ray, referral, etc
·
Other treatment:
o Sciatic pain: epidural steroid injection
o Surgery: remove disc protrusion, decompression or stabilisation
Related Topics