Chapter: Medical Physiology: The Eye: III. Central Neurophysiology of Vision
Autonomic Control of Accommodation and Pupillary Aperture
Autonomic Control of Accommodation and Pupillary Aperture
Autonomic Nerves to the Eyes. The eye is innervated byboth parasympathetic and sympathetic nerve fibers, as shown in Figure 51–11. The parasympathetic pregan-glionic fibers arise in the Edinger-Westphal nucleus (the visceral nucleus portion of the third cranial nerve) and then pass in the third nerve to the ciliary ganglion, which lies immediately behind the eye. There, the pre-ganglionic fibers synapse with postganglionic parasym-pathetic neurons, which in turn send fibers through ciliary nerves into the eyeball. These nerves excite (1)the ciliary muscle that controls focusing of the eye lens and (2) the sphincter of the iris that constricts the pupil.
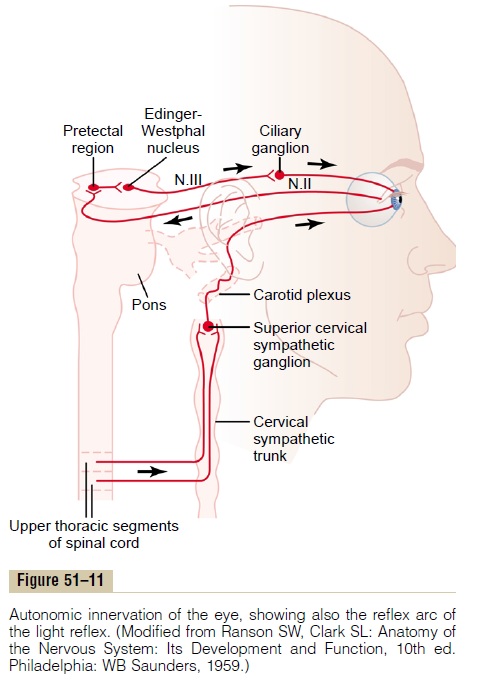
The sympathetic innervation of the eye originates in the intermediolateral horn cells of the first thoracic segment of the spinal cord. From there, sympathetic fibers enter the sympathetic chain and pass upward to the superior cervical ganglion, where they synapse with postganglionic neurons. Postganglionic sympa-thetic fibers from these then spread along the surfaces of the carotid artery and successively smaller arteries until they reach the eye. There, the sympathetic fibers innervate the radial fibers of the iris (which open the pupil) as well as several extraocular muscles of the eye, which are discussed subsequently in relation to Horner’s syndrome.
Control of Accommodation (Focusing the Eyes)
The accommodation mechanism—that is, the mecha-nism that focuses the lens system of the eye—is essen-tial for a high degree of visual acuity. Accommodation results from contraction or relaxation of the eye ciliary muscle. Contraction causes increased refractive power of the lens, and relaxation causes decreased power. How does a person adjust accommodation to keep the eyes in focus all the time?
Accommodation of the lens is regulated by a nega-tive feedback mechanism that automatically adjusts the refractive power of the lens to achieve the highest degree of visual acuity. When the eyes have been focused on some far object and must then suddenly focus on a near object, the lens usually accommodates for best acuity of vision within less than 1 second. Although the precise control mechanism that causes this rapid and accurate focusing of the eye is unclear, some of the known features are the following.
First, when the eyes suddenly change distance of the fixation point, the lens changes its strength in the proper direction to achieve a new state of focus within a fraction of a second. Second, different types of clues help to change the lens strength in the proper direction:
1. Chromatic aberration appears to be important.That is, red light rays focus slightly posteriorly to blue light rays because the lens bends blue rays more than red rays. The eyes appear to be able to detect which of these two types of rays is in better focus, and this clue relays information to the accommodation mechanism whether to make the lens stronger or weaker.
2. When the eyes fixate on a near object, the eyes must converge. The neural mechanisms for convergence cause a simultaneous signal to strengthen the lens of the eye.
3. Because the fovea lies in a hollowed-out depression that is slightly deeper than the remainder of the retina, the clarity of focus in the depth of the fovea is different from the clarity of focus on the edges. Ithas been suggested that this also gives clues about which way the strength of the lens needs to be changed.
4. It has been found that the degree ofaccommodation of the lens oscillates slightly allthe time at a frequency up to twice per second.
The visual image becomes clearer when the oscillation of the lens strength is changing in the appropriate direction and becomes poorer when the lens strength is changing in the wrong direction. This could give a rapid clue as to which way the strength of the lens needs to change to provide appropriate focus.
The brain cortical areas that control accommoda-tion closely parallel those that control fixation move-ments of the eyes, with analysis of the visual signals in Brodmann’s cortical areas 18 and 19 and transmission of motor signals to the ciliary muscle through the pretectal area in the brain stem, then through the Edinger-Westphal nucleus, and finally by way of parasympathetic nerve fibers to the eyes.
Control of Pupillary Diameter
Stimulation of the parasympathetic nerves also excites the pupillary sphincter muscle, thereby decreasing the pupillary aperture; this is called miosis. Conversely, stimulation of the sympathetic nerves excites the radial fibers of the iris and causes pupillary dilation, called mydriasis.
Pupillary Light Reflex. When light is shone into the eyes,the pupils constrict, a reaction called the pupillary lightreflex. The neuronal pathway for this reflex is demon-strated by the upper two black traces in Figure 51–11. When light impinges on the retina, a few of the result-ing impulses pass from the optic nerves to the pretec-tal nuclei. From here, secondary impulses pass to the Edinger-Westphal nucleus and, finally, back through parasympathetic nerves to constrict the sphincter of theiris. Conversely, in darkness, the reflex becomes inhib-ited, which results in dilation of the pupil.
The function of the light reflex is to help the eye adapt extremely rapidly to changing light conditions. The limits of pupillary diameter are about 1.5 millimeters on the small side and 8 millimeters on the large side. Therefore, because light brightness on the retina increases with the square of pupillary diameter, the range of light and dark adap-tation that can be brought about by the pupillary reflex is about 30 to 1—that is, up to as much as 30 times change in the amount of light entering the eye.
Pupillary Reflexes or Reactions in Central NervousSystem Disease. A few central nervous system diseases damagenerve transmission of visual signals from the retinas to the Edinger-Westphal nucleus, thus sometimes blocking the pupillary reflexes. Such blocks frequently occur as a result of central nervous system syphilis, alcoholism,encephalitis, and so forth.The block usually occurs in thepretectal region of the brain stem, although it can result from destruction of some small fibers in the optic nerves.
The final nerve fibers in the pathway through the pre-tectal area to the Edinger-Westphal nucleus are mostly of the inhibitory type. When their inhibitory effect is lost, the nucleus becomes chronically active, causing the pupils to remain mostly constricted, in addition to their failure to respond to light.
Yet the pupils can constrict a little more if the Edinger-Westphal nucleus is stimulated through some other pathway. For instance, when the eyes fixate on a near object, the signals that cause accommodation of the lens and those that cause convergence of the two eyes cause a mild degree of pupillary constriction at the same time. This is called the pupillary reaction to accommodation. A pupil that fails to respond to lightbut does respond to accommodation and is also very small (an Argyll Robertson pupil) is an important diag-nostic sign of central nervous system disease—often syphilis.
Horner’s Syndrome. The sympathetic nerves to the eye areoccasionally interrupted. Interruption frequently occurs in the cervical sympathetic chain. This causes the clini-cal condition called Horner’s syndrome, which consists of the following effects: First, because of interruption of sympathetic nerve fibers to the pupillary dilator muscle, the pupil remains persistently constricted to a smaller diameter than the pupil of the opposite eye. Second, the superior eyelid droops because it is normally main-tained in an open position during waking hours partly by contraction of smooth muscle fibers embedded in the superior eyelid and innervated by the sympathetics. Therefore, destruction of the sympathetic nerves makes it impossible to open the superior eyelid as widely as normally. Third, the blood vessels on the corresponding side of the face and head become persistently dilated. Fourth, sweating (which requires sympathetic nerve signals) cannot occur on the side of the face and head affected by Horner’s syndrome.
Related Topics