Chapter: Clinical Dermatology: Eczema and dermatitis
Atopic eczema
Atopic eczema
The
word ‘atopy’ comes from the Greek (a-topos: ‘without a place’). It was
introduced by Coca and Cooke in 1923 and refers to the lack of a niche in the
medical classifications then in use for the grouping of asthma, hay fever and
eczema. Atopy is a state in which an exuberant production of IgE occurs as a
response to common environmental allergens. Atopic subjects may, or may not,
develop one or more of the atopic diseases such as asthma, hay fever, eczema
and food allergies, and the prevalence of atopy is steadily rising.
In
Scotland, as many as 8% of children under 2 years have visible atopic eczema.
At least 1 school-child in 10 in Europe now suffers from atopic eczema and this
figure is still rising. The reasons for this are not yet clear, but are
unlikely to be a change in the genetic pool in the population. However, several
envir-onmental factors have been shown to reduce the risk of developing atopic
disease. These include having many older siblings, growing up on a farm, having
childhood measles and gut infections. The ‘hygiene hypothesis’ unites these,
blaming changes in infant diets, the early use of antibiotics and a reduced
expo-sure to orofaecal and other infections for preventing normal immunological
maturation. The subsequent understimulation of gut-associated lymphoid tissue
may predispose to atopic sensitization to environ-mental allergens. The
circulating T lymphocytes of children destined to develop allergies shift to a
type II response and are poor at
producing γ-interferon
(IFN-γ); this
persists into late childhood.Early infections may lower the risk of allergy by
boosting the production of INF-γ.
One
promising but still experimental way of tack-ling these problems has emerged
recently, involving the use of probiotics, which are cultures of potentially
beneficial bacteria. They may reverse the increased intestinal permeability
that is characteristic of children with atopic eczema. In one recent study, the
perinatal administration of a Gram-positive probiotic (Lacto-bacillus
GG) halved the subsequent occurrence ofeczema in at-risk
infants.
Inheritance
A
strong genetic component is obvious, although affected children can be born to
clinically normal parents. The concordance rates for atopic eczema in
monozygotic and dizygotic twins are 86% and 21%, respectively; and atopic
diseases tend to run true to type within each family. In some, most of the
affected members will have eczema; in others respiratory allergy will
predominate. There is also a tendency for atopic diseases to be inherited more
often from the mother than the father. Environmental factors too are import-ant
and, not surprisingly, a simple genetic explanation has not yet been found.
Probably
the inheritance of atopic eczema requires genes that predispose to the state of
atopy itself, and others that determine whether it is asthma, eczema or hay
fever that occurs. One plausible gene for the inheritance of atopy itself lies
on chromosome 11q13. It encodes for the E subunit of the high affinity IgE
receptor, which is found both on mast cells (Fig. 8.1) and on
antigen-presenting cells in the skin. However, it has to be pointed out that
several groups have failed to confirm this linkage either in the families of
those with atopic eczema or respiratory allergy. Most recently, another gene
strongly linked to atopic eczema has been found on chromosome 3q21. It encodes
for clus-ter of differentiation (CD) antigens 80 and 86. Other candidates lie
on chromosomes 14q, 16p and 17p.
Presentation and course
Seventy-five
per cent of cases of atopic eczema begin before the age of 6 months, and 80–90%
before the age of 5 years. It affects at least 3% of infants, but the onset may
be delayed until childhood or adult life. Some 60–70% of children with atopic
eczema will clear by their early teens, although subsequent relapses are
possible. The distribution and character of the lesions vary with age (Fig.
7.12) but a general dryness of the skin may persist throughout life.
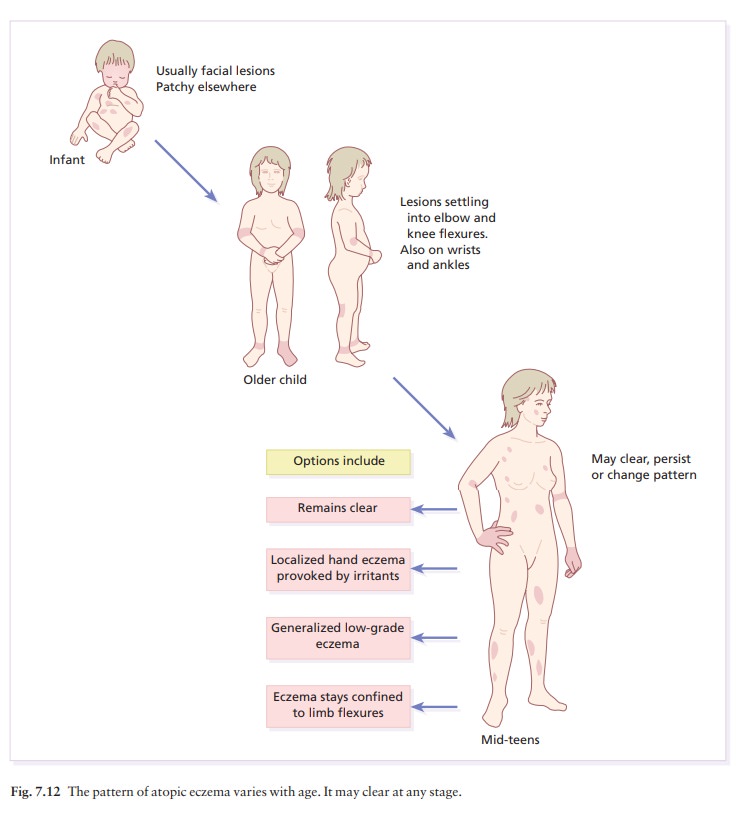
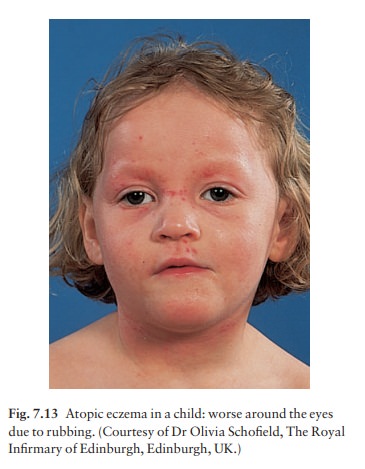
•
In infancy, atopic eczema tends to
be vesicular and weeping. It often starts on the face (Fig. 7.13) with a
non-specific distribution elsewhere, commonly spar-ing the napkin (diaper)
area.
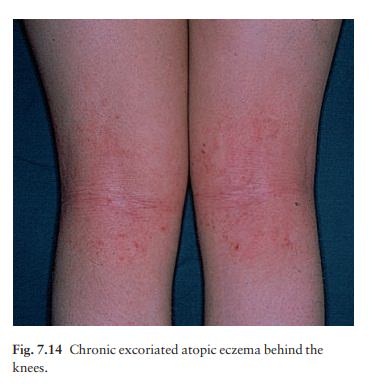
•
In childhood, the eczema becomes
leathery, dry and excoriated, affecting mainly the elbow and knee flexures
(Fig. 7.14), wrists and ankles. A stubborn ‘reverse’ pattern affecting the
extensor aspects of the limbs is also recognized.
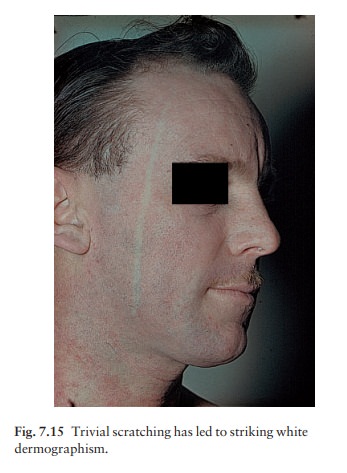
•
In adults, the distribution is as in
childhood with a marked tendency towards lichenification and a more widespread
but low-grade involvement of the trunk, face and hands. White dermographism
(Fig. 7.15) is often striking, but not diagnostic of atopic eczema.
The
cardinal feature of atopic eczema is itching; and scratching may account for
most of the clin
Affected children may sleep poorly, be hyperactive and sometimes
manipulative, using the state of their eczema to get what they want from their
parents. Luckily, the condition remits spontaneously before the age of 10 years
in at least two-thirds of affected children, although it may come back at times
of stress. Eczema and asthma may seesaw, so that while one improves the other
may get worse.
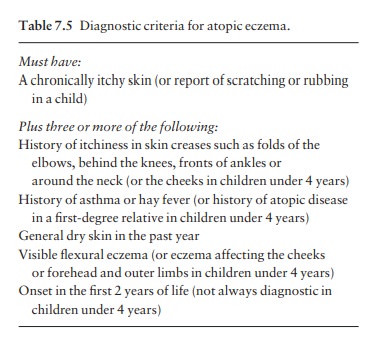
Diagnostic criteria
Useful
diagnostic criteria have been developed in the UK recently (Table 7.5).
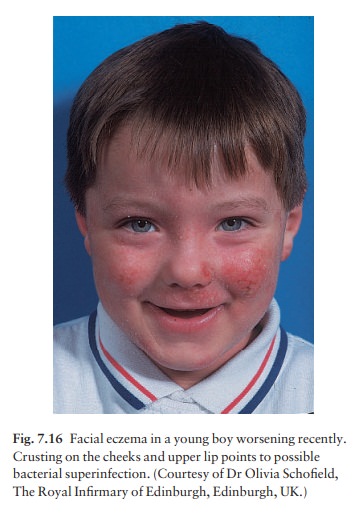
Complications
Overt bacterial infection is troublesome in many patients with atopic eczema (Fig. 7.16). They are also especially prone to viral infections, most dangerously with widespread herpes simplex (eczema herpeticum; Fig. 7.17), but also with molluscum contagiosum and warts.
Growth hormone levels
rise during deep sleep (stages 3 and 4), but these stages may not be reached
during the disturbed sleep of children with severe atopic eczema and as a
consequence they may grow poorly. The absorption of topical steroids can contribute
to this too.

Investigations
Prick
testing (see Fig. 3.10) demonstrates immediate-type hypersensitivity and is
helpful in the investigation of asthma and hay fever. However, the value of
prick testing in atopic eczema remains controversial. Often the finding of
multiple positive reactions, and a high IgE level, does little more than
support a doubtful clinical diagnosis without leading to fruitful lines of
treatment.
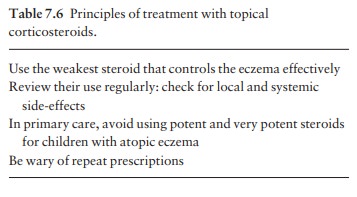
Treatment
Management
here is complex and should include the following.
•
Explanation, reassurance and
encouragement. Many patients and parents benefit from an introduction to the
National Eczema Society in the UK or the National Eczema Association for
Science and Education or the Inflammatory Skin Institute in the USA.
•
The avoidance of exacerbating
factors such as irrit-ants (e.g. woollen clothing next to the skin) and later
of careers such as hairdressing and engineering, which would inevitably lead to
much exposure to irritants. Also avoid extremes of temperature, and contact
with soaps and detergents.
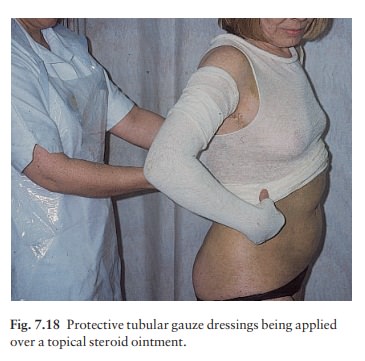
•
The judicious use of topical
steroids and other applications as for other types of chronic eczema (Table
7.6). A technique useful for extens-ive and troublesome eczema, particularly in
children, is that of ‘wet wrap’ dressingsasee above. A nurse who is expert in
applying such dressings is an asset to any practice (Fig. 7.18).
Tacrolimus is a macrolide immunosuppressant produced by a streptomycete. It is used systemically in kidney, liver and heart trans-plantation. Trials of tacrolimus in ointment form have shown that it can be a quick and highly successful topical treatment for moderate to severe atopic eczema.
The preparation seems to be safe in use, with a transient
burning sensation being the most common side-effect; however, it decreases with
usage. Some use topical steroids briefly, to improve the eczema, before
starting tacrolimus ointment, hoping in this way to decrease the incidence and
severity of this burning sen-sation. Systemic absorption is low, and skin
atrophy is not a problem. Local infection might be troublesome and the
development of skin cancer, especially on exposed treated areas, is a concern
when the drug is used for prolonged periods. Perhaps more information and
experience are required before tacrolimus can be hailed as a revolutionary new
treatment for the treatment of inflammatory skin disordersabut the results so
far look highly impressive. Topical tacrolimus is now available as Protopic
ointment.
Pimecrolimus
is another topical immunosuppressant and a derivative of askamycin. Clinical
trials in moderate atopic eczema have been encouraging and it can be used in
patients older than 3 months. Its action is very similar to that of tacrolimus
and time will tell if either preparation is superior.
•
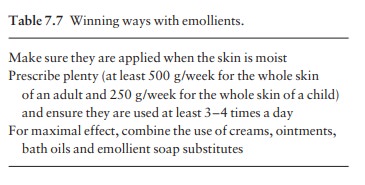
The regular use of bland emollients,
either directly to the skin or in the form of oils to be used in the bath. Some
of these can also be used as soap substitutes. A list of suitable preparations
is given in Formulary 1. Some rules governing the use of emollients are given
in Table 7.7.
•
Those with an associated ichthyosis
should gener-ally use ointments rather than creams.
• The scratch–itch cycle can often be interrupted by occlusive bandaging, e.g. with a 1% ichthammol paste bandage. Nails should be kept short.
•
Sedative antihistamines, e.g.
trimeprazine or hydro-xyzine are of
value if sleep is interrupted, but histamine release is not the main cause of
the itching, so the newer non-sedative anti-histamines help less than might be
expected.
•
Acute flares are often induced by
the surface pro-liferation of staphylococci, even without frank sepsis. A
month’s course of a systemic antibiotic, e.g. eryth-romycin, may then be
helpful.
• Allergen avoidance: prick tests confirm that most sufferers from atopic eczema have immediate hyper-sensitivity responses to allergens in the faeces of house dust mites. Sometimes, but not always, measures to reduce contact with these allergens help eczema. These measures should include encasing the mattress in a dustproof bag, washing the duvets and pillows every 3 months at a temperature greater than 55°C, and thorough and regular vacuuming in the bedroom, where carpets should preferably be avoided.
•
Do not keep pets to which there is
obvious allergy.
•
The role of diet in atopic eczema is
even more debatable, and treatments based on changing the diet of sufferers are
often disappointing. Similarly, it is not certain that the avoidance of dietary
allergens (e.g. cow’s milk and eggs) by a pregnant or lactating woman lessens
the risk of her baby developing eczema. It may still be wise to breastfeed children
at special risk for 6 months.
•
Routine inoculations are permissible
during quiet phases of the eczema. However, children who are allergic to eggs
should not be inoculated against measles, influenza and yellow fever.
•
Those with active herpes simplex infections
should be avoided to cut the risk of developing eczema herpeticum.
•
In stubborn cases UVB, UVA-1
(340–400 nm) or even PUVA therapy may be useful.
•
Cyclosporin: severe and unresponsive
cases may be helped by short courses under specialist supervision.
•
Chinese herbal remedies: properly
conducted trials have given promising results but difficulties remain. The
active ingredients within these complex mixtures of herbs have still not been
identified. We have some hope for the future but currently do not prescribe
these treatments for our patients.
Related Topics