Chapter: Clinical Cases in Anesthesia : Noncardiac Surgery After Heart Transplantation
Which immunosuppressive medications are typically used following cardiac transplantation?
Which
immunosuppressive medications are typically used following cardiac
transplantation?
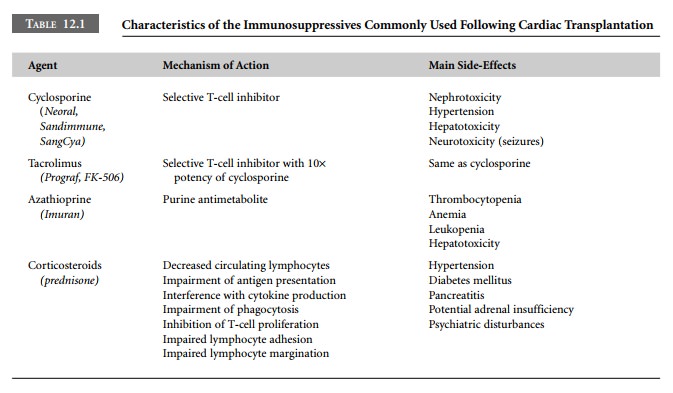
Frequently, immunosuppressive regimens consist
of selective T-cell inhibitors such as cyclosporine or tacrolimus; nonspecific
purine antimetabolites, such as azathioprine; and corticosteroids, such as
prednisone. Characteristics of these medications are summarized in Table 12.1.
Classic regimens based on high-dose steroids and multiple immunosuppressive
agents are falling out of favor, and may soon be replaced by regimens based on
rap-idly tapered steroids and tacrolimus. Other agents, includ-ing mycophenolate
mofetil (CellCept) and sirolimus (Rapamune), are approved for use following
cardiac trans-plantation, and are becoming part of typical immunosup-pressive
maintenance regimens.
While immunosuppressive agents are the key to survival following cardiac transplantation, they also have detrimental side-effects. Cyclosporine and tacrolimus tend to cause renal insufficiency, hepatotoxicity, hypertension, and neu-rotoxicity. Neurotoxicity manifests as seizures, which result from lowering the seizure threshold. Azathioprine primarily causes hematologic toxicity, producing thrombocytopenia and anemia, but also causes hepatotoxicity. Steroids can cause hypertension, diabetes mellitus, adrenal insuffi-ciency, pancreatitis, and psychiatric disturbances.
While side-effects such as those listed in
Table 12.1 may require medical management, some others mandate surgi-cal
management. These side-effects will constitute some of the most frequent
indications for non-cardiac surgery in the post-transplantation period.
Steroids predispose to peptic ulceration,
aseptic bone necrosis, and cataracts. Consequently, patients receiving chronic
high-dose steroids may present for drainage of abscesses; orthopedic procedures
on the hips, knees, elbows, or shoulders; bowel resection for perforated viscus
and diverticulitis; as well as ophthalmologic procedures related to cataracts
and retinal detachments.
Cyclosporine, tacrolimus, and azathioprine tend
to cause biliary stasis, so patients on these agents often pres-ent for
cholecystectomy. Their nonspecific gastrointestinal toxicities can also cause
severe symptoms (e.g., nausea, vomiting, diarrhea, anorexia, and abdominal
pain) mim-icking an intra-abdominal process that occasionally prompts
exploratory laparotomy.
Immunosuppression predisposes to malignancies.
Some of these patients may present for lymphoma staging, node sampling, and
resection of gynecologic or skin malignancies.
Related Topics