Chapter: Clinical Cases in Anesthesia : Noncardiac Surgery After Heart Transplantation
Explain the pre-anesthetic concerns for patients with a transplanted heart
Explain
the pre-anesthetic concerns for patients with a transplanted heart.
Preoperatively, the primary concern is the
transplanted heart’s function. Without rejection, the post-transplantation
patient generally does not perceive any functional limita-tions and is
classified as a New York Heart Association (NYHA) class I or II. However, ventricular
function must be assessed preoperatively. Information regarding prior episodes
of rejection (if any) and ventricular function is usually available from the
managing cardiologist. This is especially important in patients who are a few
years out from their transplant, because the post-cardiac transplan-tation
patient is subject to accelerated atherosclerotic coronary disease (possibly
the result of a vasculitis from low-level, subclinical rejection). The
likelihood of signifi-cant coronary occlusion increases directly with time from
transplantation. Post-transplant coronary occlusion is reported to occur at a
rate of 10–20% incidence at 1 year, 25–45% incidence at 3 years, and a 50%
incidence at 5 years.
While some benign dysrhythmias are common following
transplantation (e.g., incomplete right bundle branch block, premature atrial
contractions, occasional premature ventric-ular contractions, and first-degree
AV block), more ominous rhythms may be signs of acute rejection. Given the
propen-sity toward accelerated atherosclerotic disease, one should always
consider that new perioperative dysrhythmias accompanied by hypotension may be
a sign of ischemia.
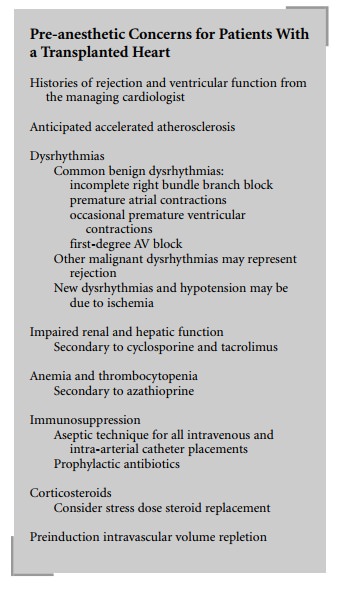
During the preoperative evaluation, special
attention should be paid to renal and hepatic function because impair-ment of
these organs is a major side-effect of the immuno-suppressive medications
cyclosporine and tacrolimus. Renal and/or hepatic impairment may predispose to
acid-base and electrolyte derangements. A complete blood count should be
reviewed for anemia and thrombocytopenia, as hemato-logic toxicity is a major
side-effect of azathioprine.
Infection is a major source of morbidity and
mortality for the immunosuppressed post-transplant patient, so aseptic
technique is mandatory for all invasive procedures, including intravenous
catheter placement. Prophylactic antibiotics are routinely employed where
appropriate.
Many immunosuppressive regimens include fairly
high dose corticosteroids, and unless the patient has recently been tapered off
steroids, the issue of a preoperative “stress dose” should be discussed with
the primary managing physician.
Finally, given the dependence of the graft on
the Frank-Starling mechanism (discussed above), one must assure an adequate
intravascular volume status prior to anesthetic induction.
Related Topics