Chapter: Clinical Cases in Anesthesia : Liver Disease
What should a preoperative evaluation of this patient include?
What should
a preoperative evaluation of this patient include?
Preoperative evaluation of patients with liver
disease focuses on symptoms of liver dysfunction. Examples are easy bruising,
bleeding problems, mental status changes, and dyspnea on exertion or at rest.
Portal hypertension predisposes to upper gastrointestinal bleeding from
esophageal varices. Additionally, portal flow obstruction can lead to the
shunting of toxins and bacteria absorbed by the gastrointestinal system
directly into the systemic circu-lation, putting these patients at increased
risk for infection and sepsis.
In evaluating the patient with a history of
liver disease, it is extremely important to note the degree of liver dam-age
and remaining function. Although no specific single test can determine liver
function, selected preoperative tests can give significant insight into the
degree of liver function remaining.
Albumin is synthesized in the liver and has a
long (20 days) half-life. Its serum levels are a result of balancing losses
against production. Factors responsible for increased loss of albumin include
massive ascites from various causes and renal disease. Decreased production can
result from poor nutritional status and decreased hepatic synthesis. Thus,
albumin levels may indicate the degree of hepatic dysfunction more in chronic
liver disease than in fulmi-nant hepatic failure.
A good laboratory indicator of liver function
in both acute and chronic liver disease is the prothrombin time (PT). It is a
measure of factors I, II, V, VII, and X. These factors are produced by the
liver and require several inter-mediate steps, which is a reflection of the
liver’s synthetic function. Not only is the PT a good test of liver function,
it is also a good prognosticator of outcome following surgery in patients with
liver disease. It should be noted that vita-min K deficiency, disseminated
intravascular coagulation, fibrinolysis, and coumadin administration all
prolong PT independently of liver disease.
Transaminases are enzymes that help transfer
amino groups from amino acids to ketoacids. In the setting of liver cell
injury, transaminases leak into the plasma increas-ing blood levels. They serve
as indicators of liver damage; however, they have significant limitations as
determinants of liver function. In advanced chronic liver disease, transaminase
levels may actually be normal or low. This is secondary to massive loss of
liver parenchymal tissue. Although they have little prognostic value,
transaminase levels are commonly followed throughout the periopera-tive course.
Just as risk of cardiac injury has been studied
in non-cardiac surgery, the risk of nonhepatic surgery in patients with
significant liver disease has also been well studied. The Child’s
classification stratifies mortality risk of portosystemic shunting in patients
with mild, moderate, or severe liver disease. Mortality ranged from 5% to 50%,
depending on the severity of the disease. This classification has been
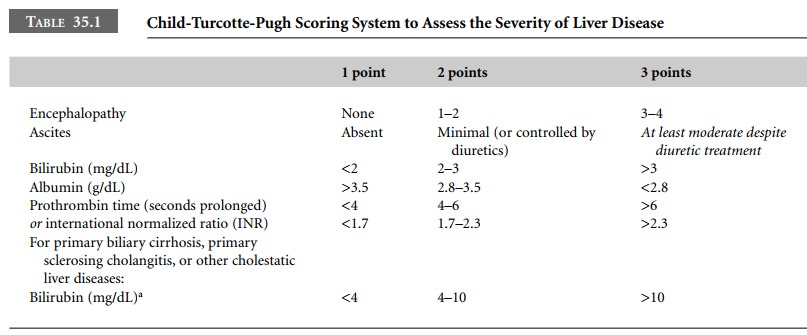
modified, the Child-Turcotte-Pugh (CTP) score (Table 35.1), which now includes
the PT and other variables. Patients with scores ≥7 are qualified to be listed for liver
transplant, whereas those with a score ≥10 are considered to have sig-nificant liver
disease.
Other useful preoperative tests would include a
hemat-ocrit, platelet count, glucose, electrolyte profile, and a blood urea
nitrogen (BUN) and creatinine. An electrocardiogram (ECG) is recommended
because of the associated cardiac problems in these patients. A detailed
physical examination of the airway, neck, heart, and lungs should be performed.
Recently, a new system was established to
improve evaluation and allocation of donor livers for patients with ESLD: the model for end-stage l iver d isease (MELD). A MELD score is
obtained based on objective and verifiable medical data that evaluates the
patient’s risk of dying while waiting for a liver transplant. This numerical
scale is currently used for liver allocation. Further information can be
obtained from the UNOS (www. unos.org/ resources).
Related Topics