Chapter: Clinical Cases in Anesthesia : Liver Disease
Describe common extrahepatic problems associated with chronic liver failure
Describe
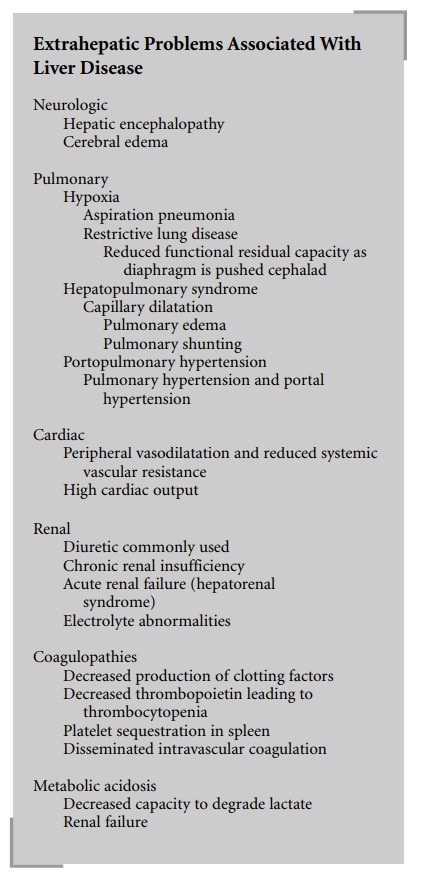
common extrahepatic problems associated with chronic liver failure.
A large number of extrahepatic problems are
associated with ESLD, which may vary widely in severity and outcome.
Neurologic Problems
Changes in mental status are common but can be
caused by a multitude of etiologies. Because there are pul-monary problems that
are associated with ESLD, one should immediately rule out hypoxia or
hypercardia as a cause for a change in mental status. Another life-threaten-ing
but easily correctable etiology is hypoglycemia. Hepatic encephalopathy is
common but not necessarily terminal. It readily responds to neomycin and
lactulose therapy. Cerebral edema, although rare, is often a preterminal event
that is associated with acute fulminant liver failure and must be treated
aggressively. Treatment consists of con-trolled mechanical hyperventilation and
administration of osmotic diuretics. Encephalopathic patients are at increased
risk for regurgitation and aspiration of gastric contents. The clinician should
have a very low threshold for elective endotracheal intubation to protect the
airway. Other causes of changes in mental status include acidosis, sepsis, and
increased side-effects of drugs secondary to increased drug levels due to
changes in pharmacokinetics. Additionally, one should always be on the lookout
for ingestion of alcohol and/or drugs by the patient.
Pulmonary Problems
Numerous pulmonary problems can occur in
patients with progressive liver disease. As mentioned previously, patients with
mental status changes are at risk for aspira-tion. Chronic cirrhotics
frequently hyperventilate due to accumulation of ammonia or acidosis.
Nevertheless, PaO2 values of 60–70 mmHg are common in these
patients. The diaphragmatic compression by massive ascites accounts for many of
the pulmonary problems encoun-tered. This effectively reduces functional
residual capacity (FRC) and predisposes to atelectasis and hypoxia. In
addi-tion, complex changes in the pulmonary arterial bed can occur. Two
clinically important and distinct pulmonary syndromes occur: hepatopulmonary
syndrome and porto-pulmonary hypertension.
Hepatopulmonary Syndrome Arterial hypoxemia associ-ate with ESLD can be
multifactorial. However, severe hypoxemia is likely secondary to
hepatopulmonary syndrome. Capillary dilatation causes a diffusion defect (a
decrease in pulmonary diffusion capacity). Additionally, right-to-left
intrapulmonary shunts may develop, leading to a noncorrectable arterial
hypoxemia. The shunts may be either secondary to atelectasis, alveoli that are
filled with fluid and/or exudate, or direct arteriovenous channels.
Portopulmonary Hypertension Pulmonary hyperten-sion is not uncommon in
advance liver disease. This can be a result of possible cardiac manifestations
of (alcohol) cirrhosis, the hyperdynamic circulation that results in high
pulmonary flows, or vasoconstriction, medial hypertrophy and intimal fibrosis
leading to potentially irreversible pulmonary hypertension. The latter, when
associated with portal hypertension, is known as portopulmonary hyper-tension
and is considered indistinguishable from primary pulmonary hypertension. It
should be noted that severe arterial hypoxemia is usually not associated with
portopul-monary hypertension.
Cardiac Problems
Cardiac disease may be difficult to diagnose in
these patients because of the debilitating nature of the liver disease. Alcohol
cirrhotics can develop a cardiomyopathy, which can lead to congestive heart
failure. However, ESLD results in massive peripheral vasodilation with a
reduced systemic vascular resistance (SVR). This effectively lowers left
ventricular work and allows for cardiac disease to exist without immediate
symptoms. A heightened suspicion for the presence of cardiac impairment is
warranted.
Patients with ESLD usually have a hyperdynamic
circula-tion that is characterized by a high cardiac output and low SVR. The
primary sites for the reduction in SVR are the splanchnic circulation and
arteriovenous shunts, which are coupled with a decrease in the viscosity of
blood secondary to anemia and the vasodilating effects of glucagon, vasoactive
intestinal peptides (VIP), substance P, and prostaglandins. The combination of
vasodilation and the formation of new arteriovenous channels results in an
increase in the intravenous compartment. Fluid retention eventually increases
the plasma volume; however, the larger increase in the intravascular
compartment with respect to the increase in plasma volume results in a relative
intravascular depletion.
Renal Problems
A host of abnormalities in renal function,
ranging from mild renal insufficiency and electrolyte imbalances to hepatorenal
syndrome, are common. Hepatorenal syn-drome usually occurs in the setting of
severe liver disease without any obvious renal etiology. Cirrhosis can be associated
with a decrease in the glomerular filtration rate (GFR) and renal blood flow
(RBF) progressing to acute oliguria. Frequent problems resulting from
aggres-sive treatment of ascites are prerenal azotemia and hypo-natremia.
Because these patients usually have relative intravascular depletion, treatment
is directed at intra-vascular volume replacement. Aggressive administration of
salt-containing solutions is unwarranted unless required to maintain
intravascular volume. Rapid correction of hyponatremia is dangerous and may
result in central pontine myelinolysis and significant neurologic injury.
The pathogenesis of hepatorenal syndrome is
incom-pletely understood. There is strong evidence to support the theory that
the relative intravascular volume depletion is a major determinant of the
initial renal hypoperfusion. Hormonal mechanisms have also been implicated. The
kidney responds to intravascular depletion by increasing renin production,
which causes constriction of the renal afferent arteries and fluid retention.
Furthermore, produc-tion of renin goes unconstrained due to the decrease in the
negative feedback from angiotensin I. In fact, patients with cirrhosis and
impaired renal functions manifest the most profound elevations of renin. The
physiologic ramifica-tions of this cycle are massive fluid retention,
electrolyte abnormalities, and a possible role in the development of
hepatorenal syndrome in ESLD.
Hematologic Problems
Other common extrahepatic problems in ESLD
include a complex coagulopathy, which is in part due to decreased synthesis of
clotting factors. Decreased production of platelets (decreased thrombopoietin),
platelet sequestra-tion by the spleen, and disseminated intravascular
coagula-tion (DIC) adversely complicate coagulation problems.
Metabolic Problems
Metabolic acidosis (metabolic alkalosis can be
seen early in the disease process), whether due to renal dysfunction or the
liver’s inability to handle lactic acid and compounds, is commonly seen in
ESLD.
Related Topics