Chapter: Clinical Cases in Anesthesia : Hypertrophic Obstructive Cardiomyopathy
What considerations should be given in planning the anesthetic management of a patient with HOCM?
What
considerations should be given in planning the anesthetic management of a
patient with HOCM?
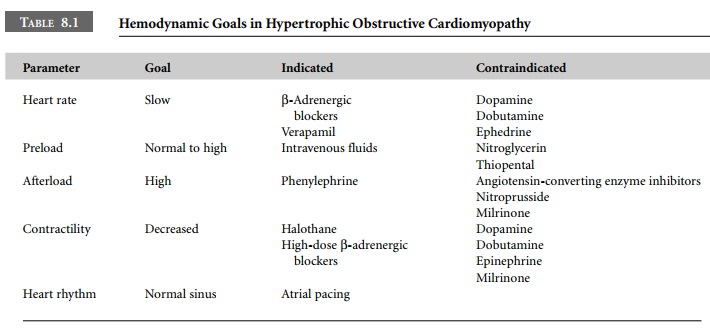
Anesthetic management of patients with HOCM
revolves around alterations in intravascular volume, ventricular contractility,
and transmural distending pressure of the outflow tract (see Table 8.1). Blood
loss, sympathectomy secondary to spinal or epidural anesthesia, nitroglycerin,
or postural changes can decrease preload. Sympathetic stimulation caused by
tracheal intubation or surgical manipulation results in an increase in
contractility and tachycardia, both of which may worsen LVOT obstruc-tion.
Inotropes, β-adrenergic agonists and calcium are con-traindicated for the same
reason. Transmural distending pressure can be decreased by hypotension
secondary to anesthetic drugs, hypovolemia, or positive-pressure venti-lation.
Tachycardia is poorly tolerated in patients with HOCM because it decreases
systolic ventricular volume thereby narrowing the outflow tract. As noted,
atrial contraction is extremely important to filling of the hypertrophied
ventricle. Therefore, nodal rhythms should be aggressively treated, using
atrial pacing if necessary.
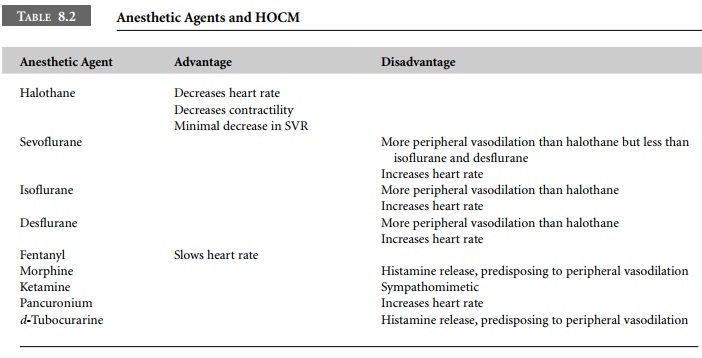
Anesthesia can be induced intravenously or by
inhala-tion of a potent anesthetic agent. Ketamine and pancuro-nium are best
avoided because of their sympathomimetic effects. Halothane is probably the
most efficacious choice if a potent volatile agent is used. Halothane decreases
heart rate and myocardial contractility, has the least effect on systemic
vascular resistance (SVR), and tends to minimize the severity of the
obstruction when volume replacement is adequate. Isoflurane and desflurane
cause pronounced peripheral vasodilation and therefore are less desirable.
Sevoflurane decreases SVR to a lesser extent, and may thus be preferable.
Agents that release histamine, such as mor-phine and d-tubocurarine, are not recommended due to the venodilation and
hypovolemia they produce. High-dose opioid anesthesia causes minimal
cardiovascular side-effects along with bradycardia, and thus may be a useful
anesthetic technique in these patients. Preoperative β-adrenergic blockade or calcium channel blocker therapy should be continued. Intravenous propranolol, meto-prolol, esmolol,
or verapamil may be administered intraoperatively to improve hemodynamic
performance (Table 8.2).
Related Topics