Chapter: Clinical Cases in Anesthesia : Cardiomyopathy Managed With A Left Ventricular Assist Device
What are the important anesthetic considerations for patients supported by LVADs?
What are
the important anesthetic considerations for patients supported by LVADs?
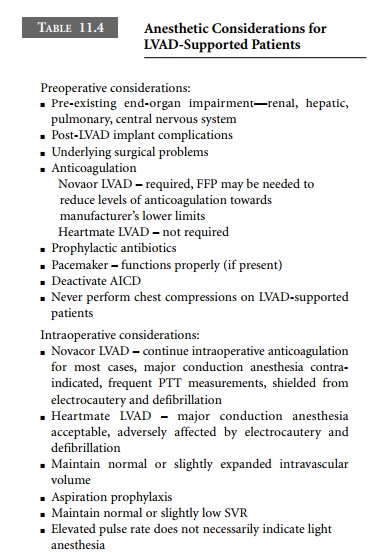
Preoperative Considerations
The preoperative clinical status of
LVAD-supported patients depends on multiple issues, such as the amount of
end-organ damage sustained during low-output states prior to ventricular assist
device (VAD) implantation, post-implantation complications, and underlying
surgical prob-lems. Many LVAD recipients are ambulatory and otherwise
uncompromised. Others experience varying degrees of renal, hepatic, pulmonary,
and/or central nervous system insufficiency. Preoperative evaluation of
neurologic dys-function and other major organ system problems is essen-tial.
Any further deterioration in the perioperative period may preclude full
recovery or disqualify a patient from later heart transplantation.
One of the most serious complications of
extracorpo-real circulation is thromboembolism, and LVADs are no exception. The
Heartmate’s blood chamber is designed with an antithrombogenic surface and
requires no formal anticoagulation; however, the Novacor’s polyurethane-lined
blood chamber mandates anticoagulation. Initially heparin is used and then
long-term warfarin therapy is commenced. International normalized ratios (INRs)
are maintained at 2.5–3.5 times normal. In elective situa-tions, Novacor
patients may discontinue warfarin therapy preoperatively and convert to
carefully monitored heparin infusions. In
most cases, heparin infusions should not be discontinued preoperatively. The majority of surgical procedures (except for neurosurgical
cases) can proceed safely in the presence of anticoagulation; however,
scrupu-lous attention to hemostasis is required intraoperatively. Fresh frozen
plasma or cryoprecipitate may be infused to decrease the level of
anticoagulation toward the lower limit of manufacturer’s recommendations.
Frequent partial thromboplastin time (PTT) measurements are important to
balance the dual potential complications of hemorrhage and thromboembolism.
Anesthesiologists must determine (perhaps in consultation with the sur-geon) a
safe anticoagulation regimen for the perioperative period.
Adherence to strict aseptic technique is
mandatory for all invasive procedures and prophylactic perioperative
antibiotics are routinely employed. Infection of an LVAD is a catastrophic
complication. They are very large foreign bodies that cannot be sterilized.
As with all critical life-support equipment in
the oper-ating room, an LVAD must be connected to a reliable power supply. Its
battery life is limited.
Preoperative considerations and practices
regarding pacemakers and AICDs are much the same in LVAD-supported patients as
in other patients. The pre-set pace-maker mode is ascertained and it is
interrogated for proper functioning. Usually, atrioventricular sequential
pacing will be in use (DDD or DOO mode), because this frequently preserves RV
output (and therefore LV filling) in these patients. Magnets should be available
in case of pacemaker malfunction. Modern pacemakers will usually convert to an
asynchronous mode (e.g., AOO, VOO, or DOO) when a magnet is applied, and should
revert to their prior programming when the magnet is removed. In any event,
pacemaker-dependent patients should have their device interrogated
postoperatively to assure proper func-tioning. Many, but not all LVAD patients
will have an AICD. Unipolar electrocautery emits a high-frequency signal that
could potentially be interpreted as ventricular fibrilla-tion, resulting in
unnecessary defibrillatory discharges. Consequently, AICDs are usually
deactivated in the imme-diate preoperative setting, assuming that a
defibrillator is immediately available. Where possible, bipolar electro-cautery
should be preferentially used. In an emergency situation, a magnet may be used
to deactivate the AICD. Most AICDs (Medtronics, St. Jude, Biotronik) will
remain deactivated as long as the magnet remains in place; however, a Guidant
AICD is permanently deactivated by application of a magnet. Removal and
subsequent reapplication of the magnet is required to reactivate a Guidant
AICD.
Cardiovascular collapse in LVAD patients is
treated with standard advanced cardiac life support (ACLS) protocols. However, one should never perform chest compressions
on a ventricular assist device
(VAD)-supported patient. Dislodgment of intracardiac cannulae will result in
imme-diate exsanguination and certain death. The Novacor is very well shielded, and will not be
affected by defibrillation or electrocautery. Unfortunately, the Heartmate may
be reset to a fixed-rate mode by electrocautery and potentially damaged by
external defibrillation. For Heartmate patients, preoperative consultation with
the physician managing the LVAD is advisable to discuss the implications of
electrocautery and external defibrillation.
Intraoperative considerations
Novacor’s requisite anticoagulation
contraindicates major conduction anesthesia, which relegates most patients to
general anesthesia. In some cases, sedation with local skin infiltration, or a
regional intravenous technique (Bier block) is appropriate. Heartmate patients
are not anticoagulated and remain potential candidates for major conduction
anes-thesia. Unfortunately, no specific recommendations exist regarding this
issue at the time of writing.
The pump’s pre-peritoneal location places the
LVAD-supported patient at increased risk for aspiration pneumoni-tis.
Consequently, “full stomach” precautions (e.g., gastric acid prophylaxis and
rapid sequence induction with cricoid pressure) should be considered.
Extubation criteria of the LVAD-supported patient are the same as in any other
patient.
The anesthetic drugs used should be appropriate
for the planned operation, and should take into account any alter-ations of
physiology resulting from insufficiency of, or prior injury to, major organ
systems. For example, it may be disadvantageous to use pancuronium or
vecuronium in the patient with renal insufficiency or biliary obstruction,
respectively. Succinylcholine may be contraindicated in patients with recent
cerebrovascular accidents. VADs do not specifically contraindicate any
particular anesthetic agents, but the anesthetic plan should consider the
poten-tially dysfunctional unassisted RV. Consequently, particular attention
should be paid to optimizing RV preload, after-load, and inotropic support as
required.
Long-term, implanted LVADs are typically set to
auto-matically eject as soon as the blood chamber is full. The faster the
device fills, the faster it pumps and the higher the pump output. Hypovolemia
results in slow pump filling, decreased LVAD output, and hypotension.
Consequently, the goal of fluid management is to maintain normal or slightly
elevated intravascular volume. Markedly increased systemic vascular resistance
(SVR) impairs forward flow, resulting in incomplete pump emptying, which leads
to stagnation of blood in the pump and increased risk of thrombosis. Therefore,
maintenance of normal or slightly low systemic vascular resistance is
desirable. Management must be individualized. Inotropes, vasodilators, and
vaso-pressors are administered to achieve optimal hemodynam-ics. LVADs
generally function well as long as there is sufficient intravascular volume to
fill the pump.
Depth of anesthesia is judged, in part, by
hemodynamic parameters. However, LVAD-supported patients may not manifest
increased pulse rates, a classic sign of light anesthe-sia. As previously
discussed, LVADs eject as soon as the blood chamber fills, and it is this rate of
ejection which constitutes the LVAD-supported patient’s pulse rate. Therefore,
the pulse rate is rarely the same as the ECG-derived heart rate. For this
reason, intraoperative tachycardia, as measured by the pulse rate, is
reflective only of the speed of LVAD filling, and not of light anesthesia.
However, while relative hyper-tension is reflective of relative volume overload
and higher pump outputs, it could also reflect heightened adrenergic activity
with increased SVR (Table 11.4). Nevertheless, lack of an acutely increased
blood pressure with surgical stimula-tion is not always a reliable indicator of
adequate depth of anesthesia in an LVAD-supported patient.
Related Topics