Chapter: Medical Physiology: Vascular Distensibility and Functions of the Arterial and Venous Systems
Veins and Their Functions
Veins and Their Functions
For years, the veins were considered to be nothing more than passageways for flow of blood to the heart, but it has become apparent that they perform other special functions that are necessary for operation of the circulation. Especially important, they are capable of constricting and enlarging and thereby storing either small or large quantities of blood and making this blood available when it is required by the remain-der of the circulation. The peripheral veins can also propel blood forward by means of a so-called venouspump, and they even help to regulate cardiac output,an exceedingly important function that is described in detail.
Venous Pressures—Right Atrial Pressure (Central Venous Pressure) and Peripheral Venous Pressures
To understand the various functions of the veins, it is first necessary to know something about pressure in the veins and what determines the pressure.
Blood from all the systemic veins flows into the right atrium of the heart; therefore, the pressure in the right atrium is called the central venous pressure.
Right atrial pressure is regulated by a balance between (1) the ability of the heart to pump blood out of the right atrium and ventricle into the lungs and (2) the tendency for blood to flow from the peripheral veins into the right atrium. If the right heart is pumpingstrongly, the right atrial pressure decreases. Con-versely, weakness of the heart elevates the right atrial pressure. Also, any effect that causes rapid inflow of blood into the right atrium from the peripheral veins elevates the right atrial pressure. Some of the factors that can increase this venous return (and thereby increase the right atrial pressure) are (1) increased blood volume, (2) increased large vessel tone through-out the body with resultant increased peripheral venous pressures, and (3) dilatation of the arterioles, which decreases the peripheral resistance and allows rapid flow of blood from the arteries into the veins.
The same factors that regulate right atrial pressure also enter into the regulation of cardiac output because the amount of blood pumped by the heart depends on both the ability of the heart to pump and the tendency for blood to flow into the heart from the peripheral vessels. Therefore, we will discuss regula-tion of right atrial pressure in much more depth in connection with regulation of cardiac output.
The normal right atrial pressure is about 0 mm Hg, which is equal to the atmospheric pressure around the body. It can increase to 20 to 30 mm Hg under very abnormal conditions, such as (1) serious heart failure or (2) after massive transfusion of blood, which greatly increases the total blood volume and causes excessive quantities of blood to attempt to flow into the heart from the peripheral vessels.
The lower limit to the right atrial pressure is usually about -3 to -5 mm Hg below atmospheric pressure. This is also the pressure in the chest cavity that sur-rounds the heart. The right atrial pressure approaches these low values when the heart pumps with excep-tional vigor or when blood flow into the heart from the peripheral vessels is greatly depressed, such as after severe hemorrhage.
Venous Resistance and Peripheral Venous Pressure
Large veins have so little resistance to blood flow whenthey are distended that the resistance then is almostzero and is of almost no importance. However, as shown in Figure 15–9, most of the large veins that enter the thorax are compressed at many points by the sur-rounding tissues, so that blood flow is impeded at these points. For instance, the veins from the arms are com-pressed by their sharp angulations over the first rib. Also, the pressure in the neck veins often falls so low that the atmospheric pressure on the outside of the neck causes these veins to collapse. Finally, veins coursing through the abdomen are often compressed by different organs and by the intra-abdominal pres-sure, so that they usually are at least partially collapsed to an ovoid or slitlike state. For these reasons, the large veins do usually offer some resistance to blood flow, and because of this, the pressure in the more
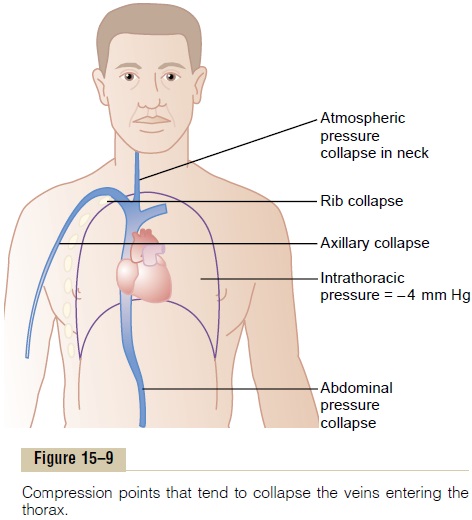
peripheral small veins in a person lying down is usually +4 to +6 mm Hg greater than the right atrial pressure.
Effect of High Right Atrial Pressure on Peripheral Venous Pres-sure. When the right atrial pressure rises above itsnormal value of 0 mm Hg, blood begins to back up in the large veins. This enlarges the veins, and even the collapse points in the veins open up when the right atrial pressure rises above +4 to +6 mm Hg. Then, as the right atrial pressure rises still further, the addi-tional increase causes a corresponding rise in periph-eral venous pressure in the limbs and elsewhere. Because the heart must be weakened greatly to cause a rise in right atrial pressure as high as +4 to +6 mm Hg, one often finds that the peripheral venous pres-sure is not noticeably elevated even in the early stages of heart failure.
Effect of Intra-abdominal Pressure on Venous Pressures of the Leg. The pressure in the abdominal cavity of a recum-bent person normally averages about +6 mm Hg, but it can rise to +15 to +30 mm Hg as a result of pregnancy, large tumors, or excessive fluid (called “ascites”) in the abdominal cavity. When the intra-abdominal pressure does rise, the pressure in the veins of the legs must rise above the abdominal pressure before the abdominal veins will open and allow the blood to flow from the legs to the heart. Thus, if the intra-abdominal pressure is +20 mm Hg, the lowest possible pressure in the femoral veins is also +20 mm Hg.
Effect of Gravitational Pressure on Venous Pressure
In any body of water that is exposed to air, the pres-sure at the surface of the water is equal to atmospheric pressure, but the pressure rises 1 mm Hg for each 13.6 millimeters of distance below the surface. This pres-sure results from the weight of the water and there-fore is called gravitational pressure orhydrostaticpressure.
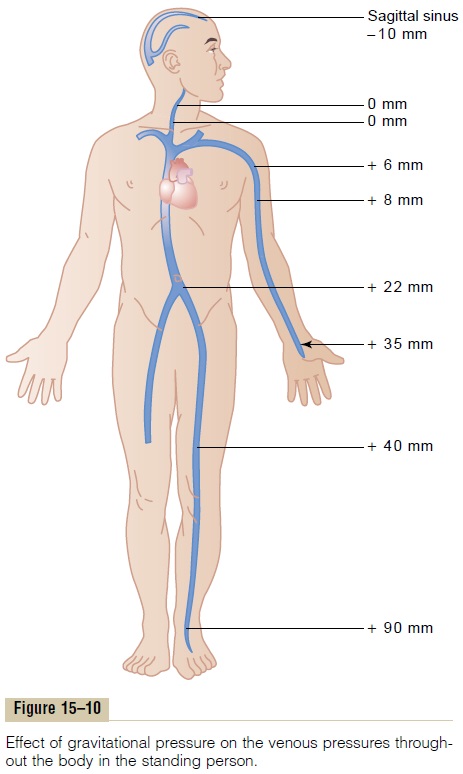
Gravitational pressure also occurs in the vascular system of the human being because of weight of the blood in the vessels, as shown in Figure 15–10. When a person is standing, the pressure in the right atrium remains about 0 mm Hg because the heart pumps into the arteries any excess blood that attempts to accu-mulate at this point. However, in an adult who is stand-ing absolutely still, the pressure in the veins of the feetis about +90 mm Hg simply because of the gravita-tional weight of the blood in the veins between the heart and the feet. The venous pressures at other levels of the body are proportionately between 0 and 90 mm Hg.
In the arm veins, the pressure at the level of the top rib is usually about +6 mm Hg because of compression of the subclavian vein as it passes over this rib. The gravitational pressure down the length of the arm then is determined by the distance below the level of this rib. Thus, if the gravitational difference between the level of the rib and the hand is +29 mm Hg, this grav-itational pressure is added to the +6 mm Hg pressure caused by compression of the vein as it crosses the rib, making a total of +35 mm Hg pressure in the veins of the hand.
The neck veins of a person standing upright collapse almost completely all the way to the skull because of atmospheric pressure on the outside of the neck. This collapse causes the pressure in these veins to remain at zero along their entire extent. The reason for this is that any tendency for the pressure to rise above this level opens the veins and allows the pressure to fall back to zero because of flow of the blood. Conversely, any tendency for the neck vein pressure to fall below zero collapses the veins still more, which further increases their resistance and again returns the pres-sure back to zero.
The veins inside the skull, on the other hand, are in a noncollapsible chamber (the skull cavity) so that they cannot collapse. Consequently, negative pressurecan exist in the dural sinuses of the head; in the stand-ing position, the venous pressure in the sagittal sinus at the top of the brain is about -10 mm Hg because of the hydrostatic “suction” between the top of the skull and the base of the skull. Therefore, if the sagittal sinus is opened during surgery, air can be sucked immedi-ately into the venous system; the air may even pass downward to cause air embolism in the heart, and death can ensue.
Effect of the Gravitational Factor on Arterial and Other Pres-sures. The gravitational factor also affects pressures inthe peripheral arteries and capillaries, in addition to its effects in the veins. For instance, a standing person who has a mean arterial pressure of 100 mm Hg at the level of the heart has an arterial pressure in the feet of about 190 mm Hg. Therefore, when one states that the arte-rial pressure is 100 mm Hg, this generally means that this is the pressure at the gravitational level of the heart but not necessarily elsewhere in the arterial vessels.
Venous Valves and the “Venous Pump”: Their Effects on Venous Pressure Were it not for valves in the veins, the gravitational pressure effect would cause the venous pressure in the feet always to be about +90 mm Hg in a standing adult. However, every time one moves the legs, one tightens the muscles and compresses the veins in or adjacent to the muscles, and this squeezes the blood out of the veins. But the valves in the veins, shown in Figure 15–11, are arranged so that the direction of venous blood flow can be only toward the heart. Conse-quently, every time a person moves the legs or even tenses the leg muscles, a certain amount of venous blood is propelled toward the heart. This pumping system is known as the “venous pump” or “muscle pump,” and it is efficient enough that under ordinary circumstances, the venous pressure in the feet of a walking adult remains less than +20 mm Hg.
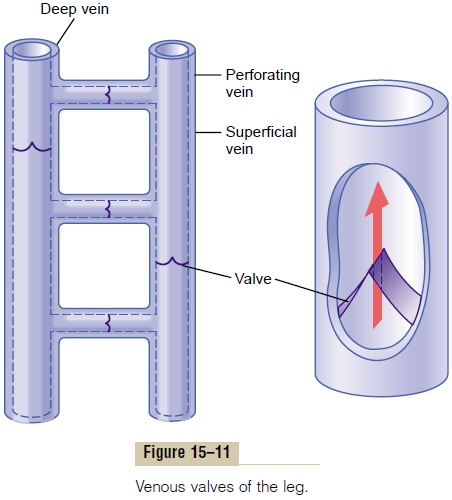
If a person stands perfectly still, the venous pump does not work, and the venous pressures in the lower legs increase to the full gravitational value of 90 mm Hg in about 30 seconds. The pressures in the capillar-ies also increase greatly, causing fluid to leak from the circulatory system into the tissue spaces. As a result, the legs swell, and the blood volume diminishes. Indeed, 10 to 20 per cent of the blood volume can be lost from the circulatory system within the 15 to 30 minutes of standing absolutely still, as often occurs when a soldier is made to stand at rigid attention.
Venous Valve Incompetence Causes “Varicose” Veins. Thevalves of the venous system frequently become “incompetent” or sometimes even are destroyed. This is especially true when the veins have been over-stretched by excess venous pressure lasting weeks or months, as occurs in pregnancy or when one stands most of the time. Stretching the veins increases their cross-sectional areas, but the leaflets of the valves do not increase in size. Therefore, the leaflets of the valves no longer close completely. When this develops, the pressure in the veins of the legs increases greatly because of failure of the venous pump; this further increases the sizes of the veins and finally destroys the function of the valves entirely. Thus, the person devel-ops “varicose veins,” which are characterized by large, bulbous protrusions of the veins beneath the skin of the entire leg, particularly the lower leg.
Whenever people with varicose veins stand for more than a few minutes, the venous and capillary pressures become very high, and leakage of fluid from the cap-illaries causes constant edema in the legs. The edema in turn prevents adequate diffusion of nutritional materials from the capillaries to the muscle and skin cells, so that the muscles become painful and weak, and the skin frequently becomes gangrenous and ulcerates. The best treatment for such a condition is continual elevation of the legs to a level at least as high as the heart. Tight binders on the legs also can be of considerable assistance in preventing the edema and its sequelae.
Clinical Estimation of Venous Pressure. The venous pressureoften can be estimated by simply observing the degree of distention of the peripheral veins—especially of the neck veins. For instance, in the sitting position, the neck veins are never distended in the normal quietly resting person. However, when the right atrial pressure be-comes increased to as much as +10 mm Hg, the lower veins of the neck begin to protrude; and at +15 mm Hg atrial pressure essentially all the veins in the neck become distended.
Direct Measurement of Venous Pressure and Right Atrial Pressure
Venous pressure can also be measured with ease by inserting a needle directly into a vein and connecting it to a pressure recorder. The only means by which rightatrial pressure can be measured accurately is by insert-ing a catheter through the peripheral veins and into the right atrium. Pressures measured through such centralvenous catheters are used almost routinely in some typesof hospitalized cardiac patients to provide constant assessment of heart pumping ability.
Pressure Reference Level for Measuring Venous and Other Circulatory Pressures
In discussions up to this point, we often have spoken of right atrial pressure as being 0 mm Hg and arterial pres-sure as being 100 mm Hg, but we have not stated the gravitational level in the circulatory system to which this pressure is referred. There is one point in the circula-tory system at which gravitational pressure factors caused by changes in body position of a healthy person usually do not affect the pressure measurement by more than 1 to 2 mm Hg. This is at or near the level of the tri-cuspid valve, as shown by the crossed axes in Figure 15–12. Therefore, all circulatory pressure measurements discussed in this text are referred to this level, which is called the reference level for pressure measurement.
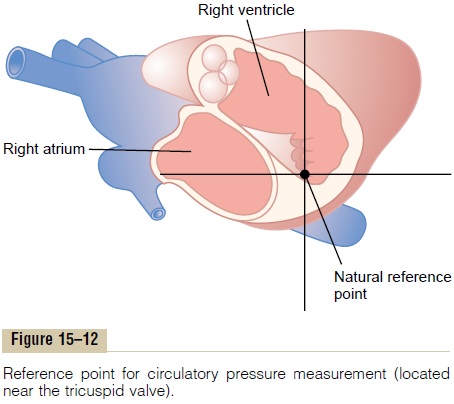
The reason for lack of gravitational effects at the tricuspid valve is that the heart automatically prevents significant gravitational changes in pressure at this point in the following way:
If the pressure at the tricuspid valve rises slightly above normal, the right ventricle fills to a greater extent than usual, causing the heart to pump blood more rapidly and therefore to decrease the pressure at the tri-cuspid valve back toward the normal mean value. Con-versely, if the pressure falls, the right ventricle fails to fill adequately, its pumping decreases, and blood dams up in the venous system until the pressure at the tricuspid level again rises to the normal value. In other words, the heart acts as a feedback regulator of pressure at thetricuspid valve.
When a person is lying on his or her back, the tricus-pid valve is located at almost exactly 60 per cent of the chest thickness in front of the back. This is the zero pres-sure reference level for a person lying down.
Blood Reservoir Function of the Veins
As pointed out, more than 60 per cent of all the blood in the circulatory system is usually in the veins. For this reason and also because the veins are so compliant, it is said that the venous system serves as ablood reservoir for the circulation.
When blood is lost from the body and the arterial pressure begins to fall, nervous signals are elicited from the carotid sinuses and other pressure-sensitive areas of the circulation. These in turn elicit nerve signals from the brain and spinal cord mainly through sympathetic nerves to the veins, causing them to constrict. This takes up much of the slack in the circulatory system caused by the lost blood. Indeed, even after as much as 20 per cent of the total blood volume has been lost, the circulatory system often functions almost normally because of this variable reservoir function of the veins.
Specific Blood Reservoirs. Certain portions of the circu-latory system are so extensive and/or so compliant that they are called “specific blood reservoirs.” These include (1) the spleen, which sometimes can decrease in size sufficiently to release as much as 100 milliliters of blood into other areas of the circulation; (2) the liver, the sinuses of which can release several hundredmilliliters of blood into the remainder of the circula-tion; (3) the large abdominal veins, which can con-tribute as much as 300 milliliters; and (4) the venousplexus beneath the skin, which also can contributeseveral hundred milliliters. The heartand the lungs, although not parts of the systemic venous reservoir system, must also be considered blood reservoirs. The heart, for instance, shrinks during sympathetic stimu-lation and in this way can contribute some 50 to 100 milliliters of blood; the lungs can contribute another 100 to 200 milliliters when the pulmonary pressures decrease to low values.
The Spleen as a Reservoir for Storing Red Blood Cells.
Figure 15–13 shows that the spleen has two separate areas for storing blood: the venous sinuses and the pulp. The sinuses can swell the same as any other partof the venous system and store whole blood.
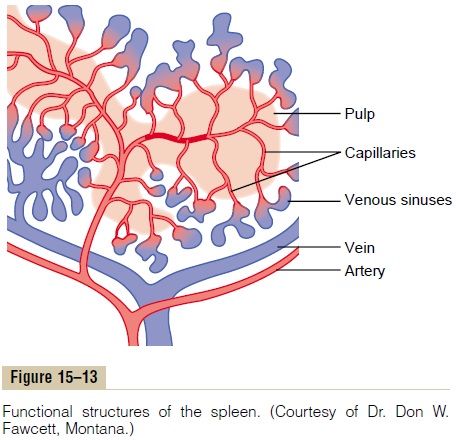
In the splenic pulp, the capillaries are so permeable that whole blood, including the red blood cells, oozes through the capillary walls into a trabecular mesh, forming the red pulp. The red cells are trapped by the trabeculae, while the plasma flows on into the venous sinuses and then into the general circulation. As a con- sequence, the red pulp of the spleen is a special reser- voir that contains large quantities of concentrated red blood cells. These can then be expelled into the general circulation whenever the sympathetic nervous system becomes excited and causes the spleen and its vessels to contract. As much as 50 milliliters of concentrated red blood cells can be released into the circulation, raising the hematocrit 1 to 2 per cent.
In other areas of the splenic pulp are islands of white blood cells, which collectively are called the white pulp.
Here lymphoid cells are manufactured similar to those manufactured in the lymph nodes. They are part of the body’s immune system.
Blood-Cleansing Function of the Spleen—Removal of Old Cells Blood cells passing through the splenic pulp before entering the sinuses undergo thorough squeezing. Therefore, it is to be expected that fragile red blood cells would not withstand the trauma. For this reason, many of the red blood cells destroyed in the body have their final demise in the spleen. After the cells rupture, the released hemoglobin and the cell stroma are digested by the reticuloendothelial cells of the spleen, and the products of digestion are mainly reused by the body as nutrients, often for making new blood cells.
Reticuloendothelial Cells of the Spleen The pulp of the spleen contains many large phagocytic lined with similar cells. These cells function as part of a cleansing system for the blood, acting in concert with a similar system of reticuloendothelial cells in the venous sinuses of the liver. When the blood is invaded by infec- tious agents, the reticuloendothelial cells of the spleen rapidly remove debris, bacteria, parasites, and so forth. Also, in many chronic infectious processes, the spleen enlarges in the same manner that lymph nodes enlarge and then performs its cleansing function even more avidly.
Related Topics