Chapter: Obstetrics and Gynecology: Pelvic Support Defects, Urinary Incontinence, and Urinary Tract Infection
Urinary Tract Infections
URINARY TRACT INFECTIONS
An
estimated 11% of U.S. women report at least one physician-diagnosed urinary tract infection (UTI) per year,
and the lifetime probability that a woman will have a UTI is 60%. Most UTIs
in women ascend from bacterial contamination of the urethra. Except in patients
with tuberculosis or in immunosuppressed patients, infections are rarely
acquired by hematogenous or lymphatic spread. The relatively short female
urethra, exposure of the meatus to vestibular and rec-tal pathogens, and sexual
activity that may induce trauma or introduce other organisms, all increase the
potential for infection (Box 28.1). Estrogen
deficiency also causes a decreasein urethral resistance to infection, which
contributes to ascending contamination. This increased susceptibility may
explain the20% prevalence of asymptomatic bacteriuria in women over the age of
65.
Of first
infections, 90% are caused by Escherichia coli.The
remaining 10% to 20% of UTIs are caused by other microorganisms, occasionally
colonizing the vagina and periurethral area. Staphylococcus saprophyticus frequently causes lower UTIs. Proteus, Pseudomonas, Klebsiella, and
Box 28.1
Risk Factors for Urinary Tract Infection
Premenopausal Women
History
of urinary tract infection
Frequent
or recent sexual activity
Diaphragm
contraception use
Use
of spermicidal agents
Increasing
parity
Diabetes
mellitus
Obesity
Sickle
cell trait
Anatomic
congenital abnormalities
Urinary
tract calculi
Neurologic
disorders or medical conditions requiring indwelling or repetitive bladder
catheterization
Postmenopausal Women
Vaginal
atrophy
Incomplete
bladder emptying
Poor
perineal hygiene
Rectocele,
cystocele, urethrocele, or uterovaginal prolapse
Lifetime
history of urinary tract infection
Type
1 diabetes mellitus
(From
American College of Obstetricians and Gynecologists. Treatment of urinary tract
infections in nonpregnant women. ACOG Practice Bulletin No. 91. Obstet Gynecol. 2008; 111(3): 785–794.)
Enterobacter
species all have been isolated in women
withcystitis or pyelonephritis, and these frequently are associ-ated with
structural abnormalities of the urinary tract, indwelling catheters, and renal
calculi. Enterococcus species also
have been isolated in women with structural abnormal-ities. Gram-positive
isolates, including group B streptococci, are increasingly isolated along with
fungal infections in women with indwelling catheters.
Clinical History
Patients with lower UTIs typically present with
symptoms of frequency, urgency, nocturia, or dysuria. The symp-toms found vary
somewhat with the site of the infection. Symptoms caused by irritation of the
bladder or trigone include urgency, frequency, and nocturia. Irritation of the
urethra leads to frequency and dysuria. Some patients may report suprapubic
tenderness or urethral or bladder-base tenderness. Fever is uncommon in women
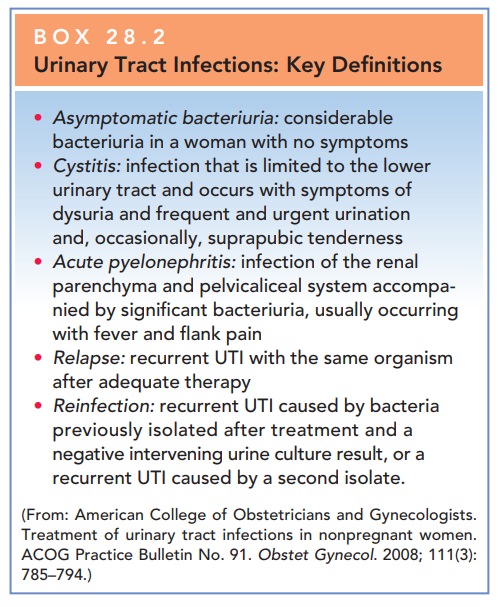
with uncompli-cated lower UTI. Upper UTI
or acute pyelonephritis fre-quently occurs with a combination of fever and
chills, flank pain, and varying degrees of dysuria, urgency, and frequency (Box
28.2).
Laboratory Evaluation
The evaluation of the patient suspected of having a uri-nary tract infection should include a urinalysis.
Box 28.2
Urinary Tract Infections: Key Definitions
Asymptomatic bacteriuria: considerablebacteriuria in a woman with no
symptoms
Cystitis: infection that is limited to the lowerurinary
tract and occurs with symptoms of dysuria and frequent and urgent urination
and, occasionally, suprapubic tenderness
Acute pyelonephritis: infection of the renalparenchyma and
pelvicaliceal system accompa-nied by significant bacteriuria, usually occurring
with fever and flank pain
Relapse: recurrent UTI with the same organismafter
adequate therapy
Reinfection: recurrent UTI caused by bacteriapreviously
isolated after treatment and a negative intervening urine culture result, or a
recurrent UTI caused by a second isolate.
(From:
American College of Obstetricians and Gynecologists. Treatment of urinary tract
infections in nonpregnant women. ACOG Practice Bulletin No. 91. Obstet Gynecol. 2008; 111(3): 785–794.)
The
initial treatment of a symptomatic lower UTI with pyuria or bacteriuria does
not require a urine culture.
However, if clinical improvement
does not occur within 48 hours or, in the case of recurrence, a urine culture
is useful to help tailor treatment.
A urine
culture should be performed in all cases of upper UTIs.
Urine for these studies is
obtained through a “clean-catch midstream” sample, which involves cleansing the
vulva and catching a portion of urine passed during the middle of uninterrupted
voiding. Urine obtained from catheters or suprapubic aspiration may also be
used. A standard uri-nalysis will detect pyuria, defined as 10 leukocytes per
milliliter, but pyuria alone is not a reliable predictor of infection. However,
pyuria and bacteriuria together on microscopic examination results markedly
increase the probability of UTI.
“Dipstick” tests for infection
based on the detection of leukocyte esterase are useful as screening tests.
However, women with negative test results and symptoms should have a urine
culture or urinalysis or both performed, because false-negative results are
common.
Cultures of urine samples that
show colony counts of more than 100,000 for a single organism generally
indi-cate infection. Colony counts as low as 10,000 for E. coli are associated with infection when symptoms are present. If
a culture report indicates multiple organisms, contami-nation of the specimen
should be suspected.
Treatment
Once infection is confirmed by
urinalysis or culture, antibiotic therapy should be instituted.
Recent
data have shown that 3 days of therapy is equivalent in efficacy to longer
durations of therapy, with eradication rates exceeding 90%.
Recommended agents for the 3-day
therapy include trimethoprim-sulfamethoxazole, trimethoprim, ciproflox-acin,
levofloxacin, and gatifloxacin.
In cases of acute pyelonephritis,
treatment should be initiated immediately. The choice of drug should be based
on knowledge of resistance in the community. Once the urine and susceptibility
culture results are available, therapy is altered as needed. Most women can be treated on an out-patient
basis initially or given intravenous fluids and one par-enteral dose of an
antibiotic before being discharged and given a regimen of oral therapy. Patients
who are severely ill, have complications, are unable to tolerate oral
medications or fluids, or who the clinician suspects will be noncompliant with
outpatient therapy should be hospitalized and receive empiric broad-spectrum
parenteral antibiotics.
Women with frequent recurrences
and prior confir-mation by diagnostic tests and who are aware of their symptoms
may be empirically treated without recurrent testing for pyuria. Management of recurrent UTIs should
startwith a search for known risk factors associated with recurrence. These
include frequent intercourse, long-term spermicide use, diaphragm use, a new
sexual partner, young age at first UTI, and a maternal history of UTI.
Behavioral changes, such as using a different form of contraception instead of
spermicide, should be advised. The first-line intervention for the prevention
of the recurrence of cystitis is prophylac-tic or intermittent antimicrobial therapy.
For women with frequent recurrences, continuous prophylaxis with once-daily
treatment with nitrofurantoin, norfloxacin, ciproflo-xacin, trimethoprim,
trimethoprim–sulfamethoxazole, or another agent has been shown to decrease the
risk of recur-rence by 95%. Drinking cranberry juice has been shown to decrease
symptomatic UTIs, but the length of therapy and the concentration required to
prevent recurrence long-term are not known.
Recurrence
is most common in postmenopausal women; the hypoestrogenic state with
associated genitourinary atrophy likely contributes to the increased
prevalence. Oral and vaginal exoge-nous estrogens have been
studied with varying results.
Screening
for and treatment of asymptomatic bacteriuria is not recommended in nonpregnant,
premenopausal women. Specific groups for whom
treatment of asymptomatic bac-teriuria is recommended include all pregnant
women, women undergoing a urologic procedure in which mucosal bleeding is
anticipated, and women in whom catheter-acquired bacteriuria persists 48 hours
after catheter removal. Treatment of asymptomatic bacteriuria in women with
diabetes mellitus, older institutionalized patients, older patients living in a
community setting, patients with spinal cord injuries, or patients with indwelling
catheters is not recommended.
Related Topics