Chapter: Obstetrics and Gynecology: Pelvic Support Defects, Urinary Incontinence, and Urinary Tract Infection
Urinary Incontinence
URINARY INCONTINENCE
The prevalence of urinary
incontinence appears to increase gradually during young adult life, has a broad
peak around middle age, and then steadily increases in the elderly. Urinary
incontinence has been shown to affect women’s social, clinical, and psychologic
well-being. It is esti-mated that less than one half of all incontinent women
seek medical care, even though the condition can often be treated.
Types
Several types of urinary
incontinence have been identified, and a patient may have more than one type
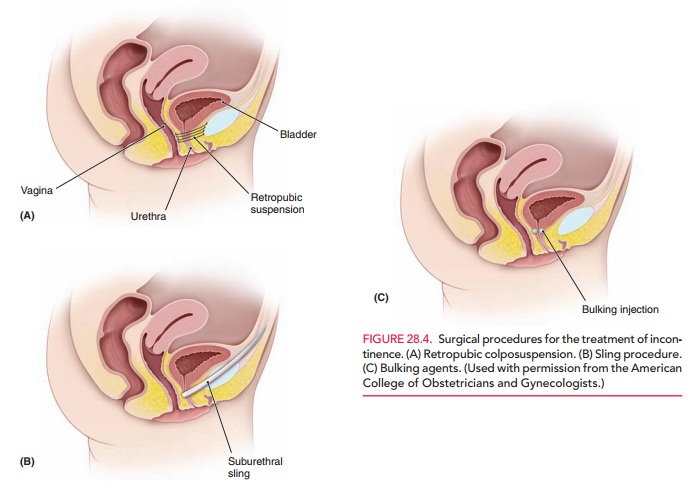
(Table 28.1).
DETRUSOR OVERACTIVITY (URGE INCONTINENCE)
The normal voiding “reflex” is
initiated when stretch receptors within the detrusor muscle, the layer of mus-cle that lines the interior
bladder wall, send a signal to the brain. The brain then decides if it is
socially acceptable to void. The detrusor muscle contracts, elevating the
blad-der pressure to exceed the urethral pressure. The external urethral
sphincter, under voluntary control, relaxes, and voiding is completed.
Normally, the detrusor muscle
allows the bladder to fill in a low-resistance setting. The volume increases
within the bladder, but the pressure within the bladder remains low. Patients
with an overactive detrusor muscle have uninhibited detrusor contractions.
These contractions cause a rise in the bladder pressure that overrides the ure-thral
pressure, and the patient will leak urine without evi-dence of increased
intra-abdominal pressure. Idiopathic detrusor overactivity has no organic
cause, but has a neuro-genic component.
A patient with detrusor overactivity presents with the feel-ing that she must run to the bathroom frequently and urgently. This may or may not be associated with nocturia. These symptoms may occur after bladder surgery to correct stress incontinence or after extensive bladder dissection during pelvic surgery.
STRESS URINARY INCONTINENCE
Normal physiology and anatomy
allow for increased abdominal pressure to be transmitted along the entire
urethra. In addition, the endopelvic fascia that extends beneath the urethra
allows for the urethra to be com-pressed against the endopelvic fascia, thus
maintaining a closed system and maintaining the bladder neck in a stable
position. In patients with stress incontinence, increased intra-abdominal
pressure is transmitted to the bladder, but not to the urethra (specifically,
the urethral–vesical junction [UVJ]), due to loss of integrity of the
endopelvic fascia. The bladder neck descends, the bladder pressure is elevated
above the intra-urethral pressure, and urine is lost. Patientswith stress incontinence present with loss of urine during
activities that cause increased intra-abdominal pressure, such as coughing,
laughing, or sneezing.
MIXED INCONTINENCE
Some
patients may have symptoms of both urge incontinence and stress incontinence. These
patients experience urine leakageduring coughing, laughing, or sneezing; the
increased intra-abdominal pressure that occurs during these activi-ties causes
the UVJ to descend and also stimulates the detrusor to contract. This clinical
scenario may be treated as stress or as detrusor instability, although it is
not clear which approach offers a better outcome.
OVERFLOW INCONTINENCE
In this form of incontinence, the
bladder does not empty completely during voiding due to an inability of the detru-sor
muscle to contract. This may occur because of an obstruction of the urethra or
a neurologic deficit that causes the patient to lose the ability to perceive
the need to void. Urine leaks out of the bladder when the bladder pressure
exceeds the urethral pressure. These
patients expe-rience continuous leakage of small amounts of urine.
Evaluation
Patients with urinary
incontinence should undergo a basic evaluation that includes a history,
physical examination, direct observation of urine loss, measurement of postvoid
residual volume, urine culture, and urinalysis. These tests and examinations
are performed to rule out urinary tract infection, neuromuscular disorders, and
pelvic support defects, all of which are associated with urinary inconti-nence.
The patient should also be asked about her fluid intake, the relationship of
her symptoms to fluid intake and activity, and medications. A voiding diary may
be helpful in this evaluation process.
Urodynamic testing may also be
useful. These tests measure the pressure and volume of the bladder as it fills
and the flow rate as it empties. In single-channel
uro-dynamic testing, the patient voids, and the volume isrecorded. A
urinary catheter is then placed and the postvoid residual (PVR) urine is
recorded. The bladder is filled in a retrograde fashion. The patient is asked
to note the first sensation that her bladder is being filled. She then is asked
to note when she has a desire to void, and when she can no longer hold her
urine. Normal values are: 100–150 cc for first sensation, 250 cc for first
desire to void, and 500–600 cc for maximum capacity. In multichannel urodynamictesting, a transducer is placed in the
vagina or rectum tomeasure intra-abdominal pressure. A transducer is placed in
the bladder, and EMG pads are placed along the per-ineum. This form of testing
provides an assessment of the entire pelvic floor, and an uninhibited bladder
contraction can be clearly documented.
Cystourethroscopy
may be used in the evaluation ofurinary
incontinence. In this procedure, a slender, lighted scope is introduced into
the bladder. Cystourethroscopy can help to identify bladder lesions and foreign
bodies, as well as urethral diverticula, fistulas, urethral strictures, and
intrinsic sphincter deficiency. It frequently is used as part of the surgical
procedures to treat incontinence.
Treatment
There are many options for
treatment. Often, treatments are more effective when used in combination.
NONSURGICAL TREATMENT OPTIONS
Lifestyle interventions that may
help modify incontinence include weight loss, caffeine reduction and fluid
manage-ment, reduction of physical forces (e.g., work, exercise), ces-sation of
smoking, and relief of constipation. Pelvic muscle training (Kegel exercises)
can be extremely effective in treat-ing some forms of incontinence, especially
stress inconti-nence. The exercises work to strengthen the pelvic floor and
thus decrease the degree of urethral hypermobility. The patient is instructed
to repeatedly tighten her pelvic floor muscles as though she were voluntarily
stopping a urine stream. Biofeedback techniques and weighted vaginal cones are
available to assist patients in learning the proper tech-nique. When performed correctly, these exercises
have success ratesof about 85%. Success is defined as a decreased number
ofepisodes of incontinence. However, once the patient stops the exercise
regimen, she will revert to her original status. Other treatments for stress
incontinence include various pessaries and continence tampons that can be
placed vagi-nally to aid in urethral compression.
Behavioral training is aimed at
increasing the patient’s bladder control and capacity by gradually increasing
the amount of time between voids. This type of training is most often used to
treat urge incontinence, but may also be successful in treating stress
incontinence and mixed incontinence. It may be augmented by biofeedback.
A number
of other pharmacologic agents appear to be effective for treating frequency,
urgency, and urge incontinence. However, the response to
treatment often is unpredictable, and side effects are common with effective
doses. Generally, drugs improve detrusor overactivity by inhibiting the
con-tractile activity of the bladder. These agents can be broadly classified
into anticholinergic agents, tricyclic antidepres-sants, musculotropic drugs,
and a variety of less commonly used drugs
Surgical Therapy
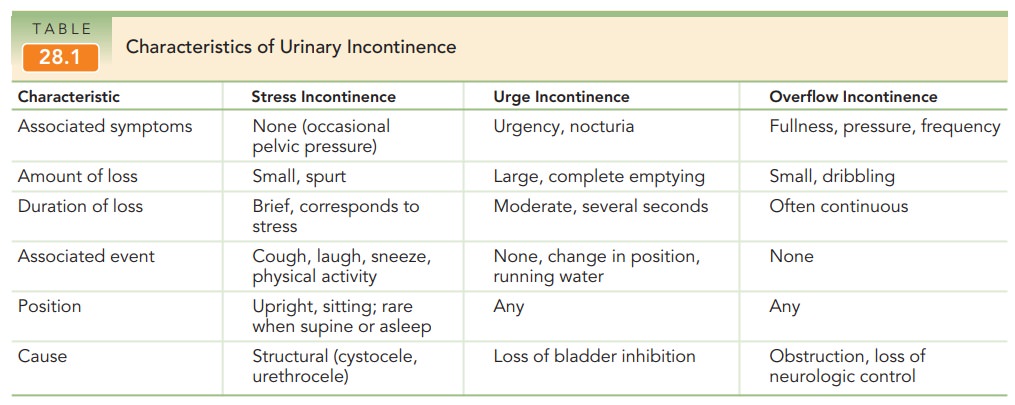
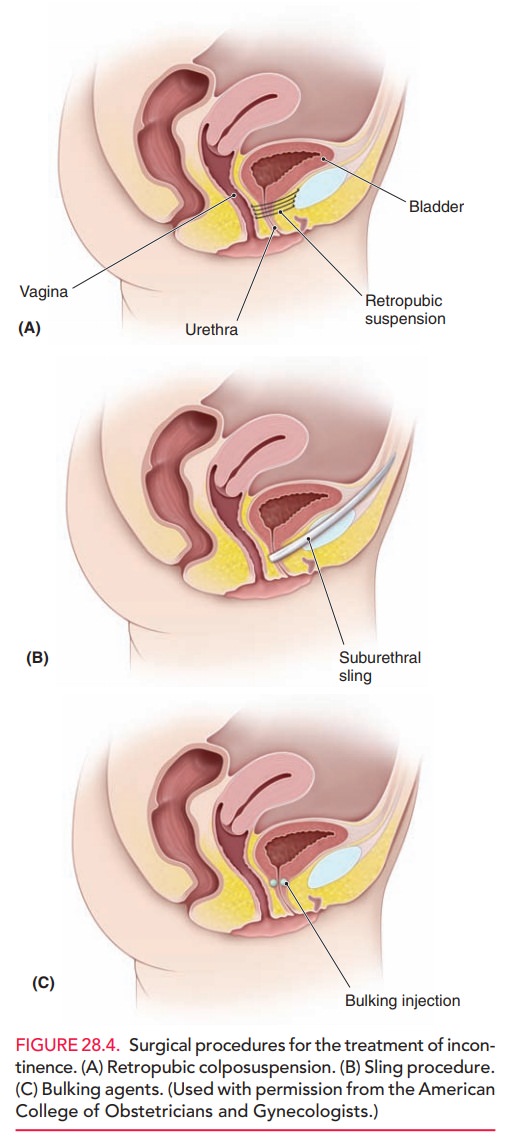
Many surgical treatments have
been developed for stress urinary incontinence, but only a few—retropubic colpo-suspension and sling procedures—have survived
andevolved with enough supporting evidence to make recom-mendations (Figs. 28.4
A and B). The aim of retropubic colposuspension is to suspend and stabilize the
anterior vaginal wall and, thus, the bladder neck and proximal urethra, in a
retropubic position. This prevents their descent and allows for urethral
compression against a sta-ble suburethral layer. In the Burch procedure, which can be performed abdominally or
laparoscopically, two or three nonabsorbable sutures are placed on each side of
the mid-urethra and bladder neck. Another procedure uses tension-free tape
placed at the midurethra to raise the urethra back into place. This procedure
can be done through the vagina. The success of tension-free vaginal tape has
led to the introduction of similar products with modified methods of
midurethral sling placement (retropubic “top-down” and transobturator). Bulking agents, such as collagen,
carbon-coated beads, and fat, are used for the treatment of urody-namic stress
incontinence with intrinsic sphincter deficiency (Fig. 28.4C). They are
injected transurethrally or peri-urethrally in the periurethral tissue around
the bladder neck and proximal urethra. They provide a “washer” effect around
the proximal urethra and the bladder neck. These agents usually are used as
second-line therapy after surgery has failed, when stress incontinence persists
with a non-mobile bladder neck, or among older, debilitated women for whom any
form of operative treatment may be hazardous.
Success rates vary depending on the skill of the surgeon and the technique used. Tension-free vaginal tape and the Burch suspension have success rate at five years of 85%. Preoperative counseling should include not only the risks of the pro-cedures, but also the goals. The patient must understand thatthe procedure may not allow her to be completely continent, as overcorrection (making the sling too tight) may lead to urinary retention. In addition, studies only show 5-year data; thus, surgery should not be presented as a permanent solu-tion. One study of women who underwent Burch colposuspensionfound that the cure rate of stress incontinence gradually decreased over 10–12 years, reaching a plateau at 69%. Approximately10% of patients required at least one additional surgery to cure their stress incontinence.
Related Topics