Chapter: Psychiatric Mental Health Nursing : Substance Abuse
Types of Substances and Treatment
TYPES OF SUBSTANCES AND TREATMENT
The classes of mood-altering substances have some similari-ties and
differences in terms of intended effect, intoxication effects, and withdrawal
symptoms. Treatment approaches after detoxification, however, are quite
similar. This section presents a brief overview of seven classes of substances
and the effects of intoxication, overdose, withdrawal, and detox-ification, and
it highlights important elements of which the nurse should be aware.
Alcohol
Intoxication and Overdose
Alcohol is a central nervous system depressant that is absorbed
rapidly into the bloodstream. Initially, the effects are relaxation and loss of
inhibitions. With intoxication, there is slurred speech, unsteady gait, lack of
coordination, and impaired attention, concentration, memory, and judg-ment.
Some people become aggressive or display inappro-priate sexual behavior when
intoxicated. The person who is intoxicated may experience a blackout.
An overdose, or excessive alcohol intake in a short period, can
result in vomiting, unconsciousness, and respiratory depression. This
combination can cause aspi-ration pneumonia or pulmonary obstruction.
Alcohol-induced hypotension can lead to cardiovascular shock and death.
Treatment of an alcohol overdose is similar to that for any central nervous
system depressant: gastric lavage or dialysis to remove the drug and support of
respi-ratory and cardiovascular functioning in an intensive care unit. The
administration of central nervous system stimu-lants is contraindicated (Lehne,
2006).
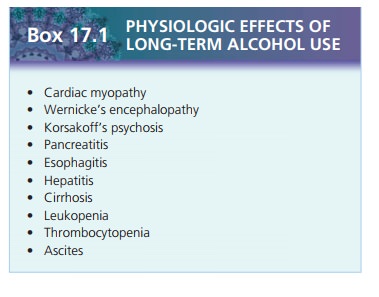
Withdrawal and Detoxification
Symptoms of withdrawal usually begin 4 to 12 hours after cessation
or marked reduction of alcohol intake. Symp-toms include coarse hand tremors,
sweating, elevated pulse and blood pressure, insomnia, anxiety, and nausea or
vomiting. Severe or untreated withdrawal may progress to transient
hallucinations, seizures, or delirium—called delirium tremens (DTs). Alcohol
withdrawal usually peaks on the second day and is over in about 5 days
(American Psychiatric Association [APA], 2000). This can vary, how-ever, and
withdrawal may take 1 to 2 weeks.
Because alcohol withdrawal can be life-threatening, detoxification
needs to be accomplished under medical supervision. If the client’s withdrawal
symptoms are mild and he or she can abstain from alcohol, he or she can be
treated safely at home. For more severe withdrawal or for clients who cannot
abstain during detoxification, a short admission of 3 to 5 days is the most
common setting. Some psychiatric units also admit clients for detoxification,
but this is less common.
Safe withdrawal is usually accomplished with the administration of
benzodiazepines such as lorazepam (Ativan), chlordiazepoxide (Librium), or
diazepam (Valium) to suppress the withdrawal symptoms. Withdrawal can be
accomplished by fixed-schedule dosing known as tapering or symptom-triggered
dosing in which the presence and severity of withdrawal symptoms determine the
amount of medication needed and the frequency of administration. Often, the
protocol used is based on an assessment tool such as the Clinical Institute
Withdrawal Assessment of Alcohol Scale. Total scores less than 8 indicate mild
withdrawal; scores from 8 to 15 indicate moderate withdrawal (marked arousal);
and scores greater than 15 indicate severe withdrawal. Clients on symptom-triggered
dosing receive medication based on scores of this scale alone, whereas clients
on fixed-dose tapers also can receive additional doses depending on the level
of scores from this scale. Both methods of medicating clients are safe and
effective.
Sedatives, Hypnotics, and Anxiolytics
Intoxication and Overdose
This class of drugs includes all central nervous system
depressants: barbiturates, nonbarbiturate hypnotics, and anxiolytics,
particularly benzodiazepines. Benzodiazepines and barbiturates are the most
frequently abused drugs in this category (Ciraulo & Sarid-Segal, 2005). The
intensity of the effect depends on the particular drug. The effects of the
drugs, symptoms of intoxication, and withdrawal symptoms are similar to those
of alcohol. In the usual pre-scribed doses, these drugs cause drowsiness and
reduce anxiety, which is the intended purpose. Intoxication symp-toms include
slurred speech, lack of coordination, unsteady gait, labile mood, impaired
attention or memory, and even stupor and coma.
Benzodiazepines alone, when taken orally in overdose, are rarely
fatal, but the person is lethargic and confused. Treatment includes gastric
lavage followed by ingestion of activated charcoal and a saline cathartic;
dialysis can be used if symptoms are severe (Lehne, 2006). The client’s
confusion and lethargy improve as the drug is excreted.
Barbiturates, in contrast, can be lethal when taken in overdose.
They can cause coma, respiratory arrest, cardiac failure, and death. Treatment
in an intensive care unit is required using lavage or dialysis to remove the
drug from the system and to support respiratory and cardiovascular function.
![]()
![]()
Withdrawal and Detoxification
The onset of withdrawal symptoms depends on the half-life of the
drug . Medications such as lora-zepam, whose actions typically last about 10
hours, pro-duce withdrawal symptoms in 6 to 8 hours; longer-acting medications
such as diazepam may not produce with-drawal symptoms for 1 week (APA, 2000).
The withdrawal syndrome is characterized by symptoms that are the oppo-site of
the acute effects of the drug: that is, autonomic hyperactivity (increased
pulse, blood pressure, respira-tions, and temperature), hand tremor, insomnia,
anxiety, nausea, and psychomotor agitation. Seizures and halluci-nations occur
only rarely in severe benzodiazepine with-drawal (Ciraulo & Sarid-Segal,
2005).
Detoxification from sedatives, hypnotics, and anxiolyt-ics is often
managed medically by tapering the amount of the drug the client receives over a
period of days or weeks, depending on the drug and the amount the client had
been using. Tapering, or
administering decreasing doses of a medication, is essential with barbiturates
to prevent coma and death that occur if the drug is stopped abruptly. For
example, when tapering the dosage of a benzodiazepine, the client may be given
Valium, 10 mg four times a day; the dose is decreased every 3 days, and the
number of times a day the dose is given also is decreased until the cli-ent
safely withdraws from the drug.
Stimulants (Amphetamines, Cocaine)
Stimulants are drugs that stimulate or
excite the central nervous system.
Although the DSM-IV-TR categorizes
amphetamines, cocaine, and central nervous system stim-ulants separately, the
effects, intoxication, and withdrawal symptoms of these drugs are virtually
identical. They are grouped together here for this reason.
Stimulants have limited clinical use (with the exception of
stimulants used to treat attention deficit hyperactivity disorder;) and a high
potential for abuse. Amphetamines (uppers) were popular in the past; they were
used by people who wanted to lose weight or to stay awake. Cocaine, an illegal
drug with virtually no clinical use in medicine, is highly addictive and a
popular recre-ational drug because of the intense and immediate feeling of
euphoria it produces.
Methamphetamine is particularly dangerous. It is highly addictive
and causes psychotic behavior. Brain damage related to its use is frequent,
primarily as a result of the substances used to make it—that is, liquid
agricul-tural fertilizer. The percentage of people admitted to inpatient
settings for methamphetamine abuse had increased in 49 of the 50 states in the
United States from 2000 to 2005. Use of methamphetamine, however, seems to have
peaked and actually declined in the past few years (Substance Abuse and Mental
Health Services Adminis-tration, 2009).
Intoxication and Overdose
Intoxication from stimulants develops rapidly; effects include the
high or euphoric feeling, hyperactivity, hyper-vigilance, talkativeness,
anxiety, grandiosity, hallucina-tions, stereotypic or repetitive behavior,
anger, fighting, and impaired judgment. Physiologic effects include
tachy-cardia, elevated blood pressure, dilated pupils, perspira-tion or chills,
nausea, chest pain, confusion, and cardiac dysrhythmias. Overdoses of
stimulants can result in sei-zures and coma; deaths are rare (Jaffe, Ling,
& Rawson, 2005). Treatment with chlorpromazine (Thorazine), an
antipsychotic, controls hallucinations, lowers blood pres-sure, and relieves
nausea (Lehne, 2006).
Withdrawal and Detoxification
Withdrawal from stimulants occurs within a few hours to several
days after cessation of the drug and is not life-threatening. Marked dysphoria
is the primary symptom and is accompanied by fatigue, vivid and unpleasant
dreams, insomnia or hypersomnia, increased appetite, and psychomotor
retardation or agitation. Marked withdrawal symptoms are referred to as
“crashing”; the person may experience depressive symptoms, including suicidal
ide-ation, for several days. Stimulant withdrawal is not treated
pharmacologically.
Cannabis (Marijuana)
Cannabis sativa is the hemp plant that is
widely cultivated for its fiber used
to make rope and cloth and for oil from its seeds. It has become widely known
for its psychoactive resin (Hall & Degenhardt, 2005). This resin contains
more than 60 substances, called cannabinoids, of which d-9-tetrahydrocannabinol is
thought to be responsible for most of the psychoactive effects. Marijuana
refers to the upper leaves, flowering tops, and stems of the plant; hashish is
the dried resinous exudate from the leaves of the female plant. Cannabis is
most often smoked in cigarettes (joints), but it can be eaten.
Cannabis is the most widely used illicit substance in the United
States. Research has shown that cannabis has short-term effects of lowering
intraocular pressure, but it is not approved for the treatment of glaucoma. It
also has been studied for its effectiveness in relieving the nausea and
vomiting associated with cancer chemotherapy and the anorexia and weight loss
of AIDS. Currently, two cannabi-noids, dronabinol (Marinol) and nabilone
(Cesamet), have been approved for treating nausea and vomiting from can-cer
chemotherapy.
Intoxication and Overdose
Cannabis begins to act less than 1 minute after inhala-tion. Peak
effects usually occur in 20 to 30 minutes and last at least 2 to 3 hours. Users
report a high feeling simi-lar to that with alcohol, lowered inhibitions,
relaxation, euphoria, and increased appetite. Symptoms of intoxica-tion include
impaired motor coordination, inappropriate laughter, impaired judgment and
short-term memory, and distortions of time and perception. Anxiety, dyspho-ria,
and social withdrawal may occur in some users. Physiologic effects, in addition
to increased appetite, include conjunctival injection (bloodshot eyes), dry
mouth, hypotension, and tachycardia. Excessive use of cannabis may produce
delirium or, rarely, cannabis-in-duced psychotic disorder, both of which are
treated symptomatically. Overdoses of cannabis do not occur (Hall &
Degenhardt, 2005).
Withdrawal and Detoxification
Although some people have reported withdrawal symp-toms of muscle
aches, sweating, anxiety, and tremors, no clinically significant withdrawal
syndrome is identified (Lehne, 2006).
Opioids
Opioids are popular drugs of abuse
because they desensi-tize the user to both physiologic and psychologic pain and
induce a sense of euphoria and well-being. Opioid com-pounds include both
potent prescription analgesics such as morphine, meperidine (Demerol), codeine,
hydromor-phone, oxycodone, methadone, oxymorphone, hydro-codone, and
propoxyphene as well as illegal substances such as heroin and normethadone.
People who abuse opi-oids spend a great deal of their time obtaining the drugs;
they often engage in illegal activity to get them. Health care professionals
who abuse opioids often write prescrip-tions for themselves or divert
prescribed pain medication for clients to themselves (APA, 2000).
Intoxication and Overdose
Opioid intoxication develops soon after the initial euphoric
feeling; symptoms include apathy, lethargy, listlessness, impaired judgment,
psychomotor retardation or agitation, constricted pupils, drowsiness, slurred
speech, and impaired attention and memory. Severe intoxication or opioid
over-dose can lead to coma, respiratory depression, pupillary con-striction,
unconsciousness, and death. Administration of naloxone (Narcan), an opioid antagonist,
is the treatment of choice because it reverses all signs of opioid toxicity.
Nalox-one is given every few hours until the opioid level drops to nontoxic;
this process may take days (Lehne, 2006).
Withdrawal and Detoxification
Opioid withdrawal develops when drug intake ceases or decreases
markedly, or it can be precipitated by the admin-istration of an opioid
antagonist. Initial symptoms are anxi-ety, restlessness, aching back and legs,
and cravings for more opioids (Jaffe & Strain, 2005). Symptoms that develop
as withdrawal progresses include nausea, vomiting, dysphoria, lacrimation,
rhinorrhea, sweating, diarrhea, yawning, fever, and insomnia. Symptoms of
opioid withdrawal cause sig-nificant distress but do not require pharmacologic
interven-tion to support life or bodily functions. Short-acting drugs such as
heroin produce withdrawal symptoms in 6 to 24 hours; the symptoms peak in 2 to
3 days and gradually sub-side in 5 to 7 days. Longer-acting substances such as
metha-done may not produce significant withdrawal symptoms for 2 to 4 days, and
the symptoms may take 2 weeks to subside. Methadone can be used as a
replacement for the opioid, and the dosage is then decreased over 2 weeks.
Substitution of methadone during detoxification reduces symptoms to no worse
than a mild case of flu (Lehne, 2006). Withdrawal symptoms such as anxiety,
insomnia, dysphoria, anhedonia, and drug craving may persist for weeks or
months.
Hallucinogens
Hallucinogens are substances that distort
the user’s percep-tion of reality and produce symptoms similar to psychosis,
including hallucinations (usually visual) and depersonal-ization. Hallucinogens
also cause increased pulse, blood pressure, and temperature; dilated pupils;
and hyperreflexia. Examples of hallucinogens are mescaline, psilocybin,
lyser-gic acid diethylamide, and “designer drugs” such as Ecstasy. PCP,
developed as an anesthetic, is included in this section because it acts
similarly to hallucinogens.
Intoxication and Overdose
Hallucinogen intoxication is marked by several maladap-tive
behavioral or psychologic changes: anxiety, depression, paranoid ideation,
ideas of reference, fear of losing one’s mind, and potentially dangerous
behavior such as jumping ![]()
![]() out a window in the belief that one can fly
(Jones, 2005). Physiologic symptoms include sweating, tachycardia,
pal-pitations, blurred vision, tremors, and lack of coordination. PCP
intoxication often involves belligerence, aggression, impulsivity, and
unpredictable behavior.
out a window in the belief that one can fly
(Jones, 2005). Physiologic symptoms include sweating, tachycardia,
pal-pitations, blurred vision, tremors, and lack of coordination. PCP
intoxication often involves belligerence, aggression, impulsivity, and
unpredictable behavior.
Toxic reactions to hallucinogens (except PCP) are primar-ily
psychologic; overdoses as such do not occur. These drugs are not a direct cause
of death, although fatalities have occurred from related accidents, aggression,
and suicide. Treatment of toxic reactions is supportive. Psychotic reactions
are managed best by isolation from external stimuli; physical restraints may be
necessary for the safety of the client and others. PCP toxic-ity can include
seizures, hypertension, hyperthermia, and respiratory depression. Medications
are used to control sei-zures and blood pressure. Cooling devices such as
hyper-thermia blankets are used, and mechanical ventilation is used to support
respirations (Lehne, 2006).
Withdrawal and Detoxification
No withdrawal syndrome has been identified for halluci-nogens,
although some people have reported a craving for the drug. Hallucinogens can
produce flashbacks, which are transient recurrences of perceptual disturbances
like those experienced with hallucinogen use. These episodes occur even after
all traces of the hallucinogen are gone and may persist for a few months up to
5 years.
Inhalants
Inhalants are a diverse group of drugs
that include anes-thetics, nitrates, and organic solvents that are inhaled for
their effects. The most common substances in this category are aliphatic and
aromatic hydrocarbons found in gasoline, glue, paint thinner, and spray paint.
Less frequently used halogenated hydrocarbons include cleaners, correction
fluid, spray can propellants, and other compounds contain-ing esters, ketones,
and glycols (APA, 2000). Most of the vapors are inhaled from a rag soaked with
the compound, from a paper or plastic bag, or directly from the container.
Inhalants can cause significant brain damage, peripheral nervous system damage,
and liver disease.
Intoxication and Overdose
Inhalant intoxication involves dizziness, nystagmus, lack of
coordination, slurred speech, unsteady gait, tremor, muscle weakness, and
blurred vision. Stupor and coma can occur. Significant behavioral symptoms are
belliger-ence, aggression, apathy, impaired judgment, and inability to
function. Acute toxicity causes anoxia, respiratory depression, vagal
stimulation, and dysrhythmias. Death may occur from bronchospasm, cardiac
arrest, suffocation, or aspiration of the compound or vomitus (Crowley &
Sakai, 2005). Treatment consists of supporting respiratory and cardiac
functioning until the substance is removed from the body. There are no
antidotes or specific medica-tions to treat inhalant toxicity.
Withdrawal and Detoxification
There are no withdrawal symptoms or detoxification pro-cedures for
inhalants as such, although frequent users report psychologic cravings. People
who abuse inhalants may suffer from persistent dementia or inhalant-induced
disorders such as psychosis, anxiety, or mood disorders even if the inhalant
abuse ceases. These disorders are all treated symptomatically (Crowley &
Sakai, 2005).
Related Topics