Chapter: Psychiatric Mental Health Nursing : Substance Abuse
Application of the Nursing Process - Substance Abuse
![]()
![]() APPLICATION OF
THE NURSING PROCESS
APPLICATION OF
THE NURSING PROCESS
Identifying people with substance use problems can be dif-ficult.
Substance use typically includes the use of defense mechanisms, especially denial. Clients may deny directly
having any problems or may minimize the extent of prob-lems or actual substance
use. In addition, the nurse may encounter clients with substance problems in
various set-tings unrelated to mental health. A client may come to a clinic for
treatment of medical problems related to alcohol use, or a client may develop
withdrawal symptoms while in the hospital for surgery or an unrelated
condition. The nurse must be alert to the possibility of substance use in these
situations and be prepared to recognize their exis-tence and to make
appropriate referrals.
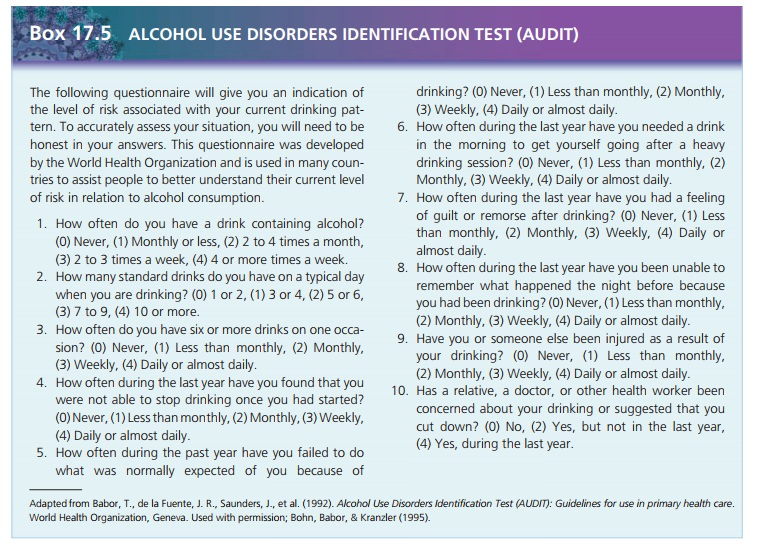
The Alcohol Use Disorders Identification Test (AUDIT) is a useful
screening device to detect hazardous drinking patterns that may be precursors
to full-blown substance use disorders (Bohn, Babor, & Kranzler, 1995). This
tool promotes recognition of problem drinking in the early stage, when
resolution without formal treatment is more likely. Early detection and
treatment are associated with more positive outcomes.
Detoxification is the initial priority. Priorities for individual
clients are based on their physical needs and may include safety, nutrition,
fluids, elimination, and sleep. The remainder of this sec-tion focuses on care
of the client being treated for sub-stance abuse after detoxification.
Assessment
History
Clients with a parent or other family members with sub-stance abuse
problems may report a chaotic family life, although this is not always the
case. They generally describe some crisis that precipitated entry into
treatment, such as physical problems or development of withdrawal symptoms
while being treated for another condition. Usu-ally, other people such as an
employer threatening loss of a job or a spouse or partner threatening loss of a
relation-ship are involved in a client’s decision to seek treatment. Rarely do
clients decide to seek treatment independently with no outside influence.
General Appearance and Motor Behavior
Assessment of general appearance and behavior usually reveals
appearance and speech to be normal. Clients may appear anxious, tired, and
disheveled if they have just completed a difficult course of detoxification.
Depending on their overall health status and any health problems resulting from
substance use, clients may appear physi-cally ill. Most clients are somewhat
apprehensive about treatment, resent being in treatment, or feel pressured by
others to be there. This may be the first time in a long time that clients have
had to deal with any difficulty without the help of a psychoactive substance.
Mood and Affect
Wide ranges of mood and affect are possible. Some clients are sad
and tearful, expressing guilt and remorse for their behavior and circumstances.
Others may be angry and sar-castic or quiet and sullen, unwilling to talk to
the nurse. Irritability is common because clients are newly free of substances.
Clients may be pleasant and seemingly happy, appearing unaffected by the
situation, especially if they are still in denial about the substance use.
Thought Process and Content
During assessment of thought process and content, clients are
likely to minimize their substance use, blame others for their problems, and
rationalize their behavior. They may believe they cannot survive without the substance
or may express no desire to do so. They may focus their atten-tion on finances,
legal issues, or employment problems as the main source of difficulty rather
than their substance use. They may believe that they could quit “on their own”
if they wanted to, and they continue to deny or minimize the extent of the
problem.
Sensorium and Intellectual Processes
Clients generally are oriented and alert unless they are
experiencing lingering effects of withdrawal. Intellectual abilities are intact
unless clients have experienced neuro-logic deficits from long-term alcohol use
or inhalant use.
Judgment and Insight
Clients are likely to have exercised poor judgment, espe-cially
while under the influence of the substance. Judg-ment may still be affected:
clients may behave impulsively such as leaving treatment to obtain the
substance of choice. Insight usually is limited regarding substance use.
Clients may have difficulty acknowledging their behavior while using or may not
see loss of jobs or relationships as con-nected to the substance use. They may
still believe they can control the substance use.
Self-Concept
Clients generally have low self-esteem, which they may express
directly or cover with grandiose behavior. They do not feel adequate to cope
with life and stress without the substance and often are uncomfortable around
others when not using. They often have difficulty identifying and expressing
true feelings; in the past, they have preferred to escape feelings and to avoid
any personal pain or difficulty with the help of the substance.
Roles and Relationships
Clients usually have experienced many difficulties with social,
family, and occupational roles. Absenteeism and poor work performance are
common. Often, family mem-bers have told these clients that the substance use
was a concern, and it may have been the subject of family argu-ments.
Relationships in the family often are strained. Cli-ents may be angry with
family members who were instru-mental in bringing them to treatment or who
threatened loss of a significant relationship.
Physiologic Considerations
Many clients have a history of poor nutrition (using rather than
eating) and sleep disturbances that persist beyond detoxification. They may
have liver damage from drink-ing alcohol, hepatitis or HIV infection from
intravenous drug use, or lung or neurologic damage from using inhalants.
Data Analysis
Each client has nursing diagnoses specific to his or her physical
health status. These may include the following:
·
Imbalanced Nutrition: Less Than Body Requirements
·
Risk for Infection
·
Risk for Injury
·
Diarrhea
·
Excess Fluid Volume
·
Activity Intolerance
·
Self-Care Deficits
Nursing diagnoses commonly used when working with clients with
substance use include the following:
·
Ineffective Denial
·
Ineffective Role Performance
·
Dysfunctional Family Processes: Alcoholism
·
Ineffective Coping
Outcome Identification
Treatment outcomes for clients with substance use may include the
following:
·
The client will abstain from alcohol and drug use.
·
The client will express feelings openly and directly.
·
The client will verbalize acceptance of responsibility for his or
her own behavior.
·
The client will practice nonchemical alternatives to deal with
stress or difficult situations.
The client will establish an effective after-care plan.
Intervention
Providing Health Teaching for Client and Family
Clients and family members need facts about the sub-stance, its
effects, and recovery. The nurse must dispel the following myths and
misconceptions:
·
“It’s a matter of will power.”
·
“I can’t be an alcoholic if I only drink beer or if I only drink on
weekends.”
·
“I can learn to use drugs socially.”
·
“I’m okay now; I could handle using once in a while.”
Education about relapse is important. Family members and friends
should be aware that clients who begin to revert to old behaviors, return to
substance-using acquain-tances, or believe they can “handle myself now” are at
high risk for relapse, and loved ones need to take action. Whether a client
plans to attend a self-help group or has other resources, a specific plan for
continued support and involvement after treatment increases the client’s
chances for recovery.
Addressing Family Issues
Alcoholism (and other substance abuse) often is called a family
illness. All those who have a close relationship with a person who abuses
substances suffer emotional, social, and sometimes physical anguish.
Codependence is a maladaptive coping
pattern on the part of family
members or others that results from a pro-longed relationship with the person
who uses substances. Characteristics of codependence are poor relationship
skills, excessive anxiety and worry, compulsive behaviors, and resistance to
change. Family members learn these dys-functional behavior patterns as they try
to adjust to the behavior of the substance user. One type of codependent
behavior is called enabling, which is a behavior that seems helpful on the
surface but actually perpetuates the sub-stance use. For example, a wife who
continually calls in to report that her husband is sick when he is really drunk
or hungover prevents the husband from having to face the true implications and
repercussions of his behavior. What appears to be a helpful action really just
assists the hus-band to avoid the consequences of his behavior and to continue
abusing the substance.
Roles may shift dramatically, such as when a child actu-ally looks
out for or takes care of a parent. Codependent behaviors also have been
identified in health care profes-sionals when they make excuses for a client’s
behavior or do things for clients that clients can do for themselves.
An adult child of an alcoholic is someone who was raised in a
family in which one or both parents were addicted to alcohol and who has been
subjected to the many dysfunctional aspects associated with parental
alco-holism. In addition to being at high risk for alcoholism and eating
disorders, children of alcoholics often develop an inability to trust, an
extreme need to control, an excessive sense of responsibility, and denial of feelings;
these charac-teristics persist into adulthood. Many people growing up in homes
with parental alcoholism believe their problems will be solved when they are
old enough to leave and escape the situation. They may begin to have problems
in relation-ships, low self-esteem, and excessive fears of abandonment or
insecurity as adults. Never having experienced normal family life, they may
find that they do not know what “nor-mal” is (Kearns-Bodkin & Leonard,
2008).
Without support and help to understand and cope, many family
members may develop substance abuse prob-lems of their own, thus perpetuating
the dysfunctional cycle. Treatment and support groups are available to address
the issues of family members. Clients and family also need information about support
groups, their pur-pose, and their locations in the community.
Promoting Coping Skills
Nurses can encourage clients to identify problem areas in their
lives and to explore the ways that substance use may have intensified those
problems. Clients should not believe that all life’s problems will disappear
with sobriety; rather, sobriety will assist them to think about the problems
clearly. The nurse may need to redirect a client’s attention to his or her
behavior and how it influenced his or her problems. The nurse should not allow
clients to focus on external events or other people without discussing their
role in the problem.
Nurse: “Can you describe some problems you’ve been having?”
Client: “My wife is always nagging—noth-ing is ever good enough—so we don’t
get along very well.”
Nurse: “How do you communicate with your wife?”
Client: “I can’t talk to her about anything; she won’tNurse: “Are you saying that you don’t talk to her very much?”
It may be helpful to role-play situations that clients have found
difficult. This is also an opportunity to help clients learn to solve problems
or to discuss situations with others calmly and more effectively. In the group
set-ting in treatment, it is helpful to encourage clients to give and to
receive feedback about how others perceive their interaction or ability to
listen.
The nurse also can help clients to find ways to relieve stress or
anxiety that do not involve substance use. Relax-ing, exercising, listening to
music, or engaging in activities may be effective. Clients also may need to
develop new social activities or leisure pursuits if most of their friends or
habits of socializing involved the use of substances.
The nurse can help clients to focus on the present, not the past.
It is not helpful for clients to dwell on past prob-lems and regrets. Rather,
they must focus on what they can do now regarding their behavior or
relationships. Clients may need support from the nurse to view life and
sobriety in feasible terms—taking it one day at a time. The nurse can encourage
clients to set attainable goals such as, “What can I do today to stay sober?”
instead of feeling over-whelmed by thinking “How can I avoid substances for the
rest of my life?” Clients need to believe that they can succeed.
Evaluation
The effectiveness of substance abuse treatment is based heavily on
the client’s abstinence from substances. In addi-tion, successful treatment
should result in more stable role performance, improved interpersonal
relationships, and increased satisfaction with quality of life.
Related Topics