Chapter: Essentials of Psychiatry: Substance Abuse: Alcohol Use Disorders
Treatment - Alcohol Use Disorders
Treatment
Goals, Setting and Costs of Treatment
When a determination has been made that an
individual is drink-ing excessively, the nature, setting and intensity of the
interven-tion must be determined in order to address the specific treatment
needs of the patient. Among heavy drinkers without evidence of alcohol
dependence, a brief intervention aimed at the reduction of drinking may
suffice. In contrast, among alcoholics, there are typically a variety of
associated disabilities, so it is necessary to address both the excessive
drinking and problems related to it.
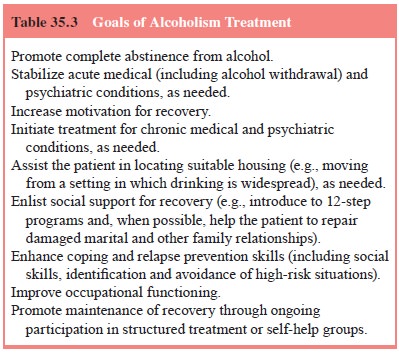
Consequently, alcoholism treatment is best conceived of as mul-timodal. Table
35.3 provides an overview of the goals of alcohol-ism treatment. It should be
noted that while total abstinence is a primary goal of treatment for persons
with alcohol dependence, moderate drinking can be considered as a goal for
persons with alcohol abuse.
Figure 35.1 describes a process for the management
of patients with alcohol abuse and dependence. The algorithm is written from
the perspective of a community-based or consul-tation/liaison psychiatrist who
does not necessarily have spe-cialized training in addiction medicine.
Following the initial
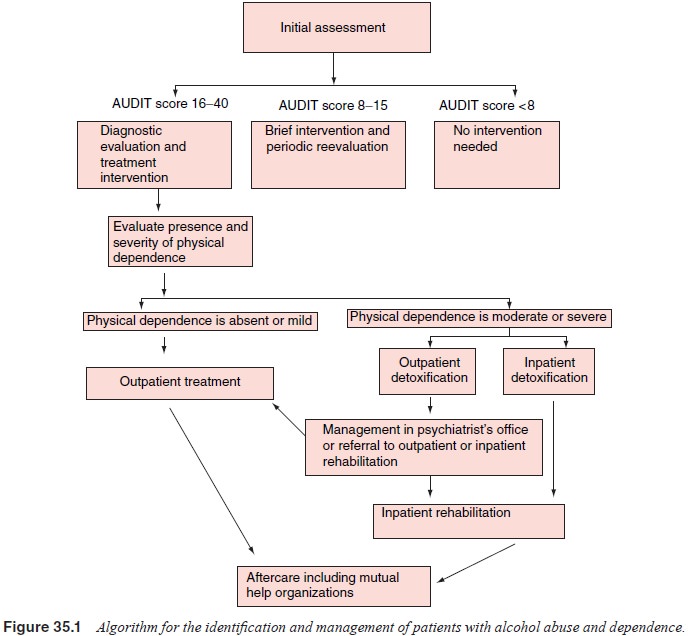
assessment, using a screening test like the CAGE or
AUDIT, the patient is referred to either a diagnostic evaluation with a likely
treatment recommendation or a brief intervention with further monitoring. Brief
interventions are characterized by their low intensity and short duration. They
typically consist of one to three sessions of counseling and education. They
are intended to provide early intervention, before or soon after the onset of
alco-hol-related problems. Brief interventions seek to motivate high risk
drinkers to moderate their alcohol consumption, rather than promote total
abstinence with specialized treatment techniques. They are simple enough to be
delivered by primary care prac-titioners and are especially appropriate for
psychiatric patients whose at-risk drinking meets criteria for alcohol abuse
rather than dependence.
If the patient’s screening results and diagnostic
evaluation provide evidence of alcohol dependence, the next step is to
differ-entiate between mild and more severe levels of physical depend-ence to
determine the need for detoxification. If withdrawal risk is low, the patient
may be referred directly to outpatient therapy. If the withdrawal risk is
moderate or high, outpatient or inpatient detoxification is indicated.
There are a number of potentially life-threatening
condi-tions for which alcoholics are at increased risk. The presence of any of
the following requires immediate attention: acute alco- hol withdrawal (with
the potential for seizures and delirium tre-mens), serious medical or surgical
disease (e.g., acute pancreati-tis, bleeding esophageal varices) and serious
psychiatric illness (e.g., psychosis, suicidal intent). In the presence of any
of these emergent conditions, acute stabilization should be the first prior-ity
of treatment.
The presence of complicating medical or psychiatric
con-ditions is an important determinant of whether detoxification and
rehabilitation are initiated in an inpatient or an outpatient setting. Other
considerations are the alcoholic’s current living circum-stances and social
support network. Women with children are sometimes unwilling to enter
residential treatment unless their family needs are taken care of. Homeless
people may be eager to enter residential treatment even when their medical or
psychiat-ric condition does not warrant it.
In the alcoholic patient whose condition is
stabilized or in the patient without these complicating features, the major
focus should be on the establishment of a therapeutic alli-ance, which provides
the context within which rehabilitation can occur. The presence of a trusting
relationship facilitates the patient’s acknowledgement of alcohol-related
problems and encourages open consideration of different treatment op-tions. In
addition to participation in structured rehabilitation treatment, the patient
should be made aware of the widespread availability of Alcoholics Anonymous
(AA) and the wide di-versity of its membership.
Residential settings include hospital-based
rehabilitation programs, freestanding units and psychiatric units. With the
growth of managed care in the 1990s, there has been a dramatic reduction in the
average length of stay for residential treatment and a shift in emphasis to
less costly outpatient treatment set-tings. There is no consistent evidence
that intensive or inpatient residential treatment provides more benefit than
less intensive outpatient treatment, but for certain kinds of patients
residential treatment may have advantages (Finney and Monahan, 1996). In many
populations, outpatient programs produce results compara-ble to those of
inpatient programs.
Another approach to patient placement and treatment
matching is based on the notion that patients should initially be matched to
the least intensive level of care that is appropriate, and then stepped up to
more intensive treatment settings if they do not respond.
Despite treatment, some alcoholics relapse
repeatedly. For many emergency department personnel, the multiple recidivist
al-coholic has come to personify the disorder. For clinicians involved in the
delivery of alcoholism rehabilitation services, these individ-uals’ apparent
unresponsiveness to treatment may contribute to frustration and a sense of
futility. Presently, long-term residential treatment appears to be the only
option for alcoholics who do not respond to more limited efforts at
rehabilitation. Unfortunately, the availability of such care in many states is
limited as a conse-quence of the effort to deinstitutionalize psychiatric
patients.
Finally, the importance of continuing care by means
of af-tercare groups, and other mutual help organizations cannot be
overestimated.
Related Topics