Chapter: Medical Surgical Nursing: Intraoperative Nursing Management
The Surgical Team
The Surgical Team
The surgical team consists of the
patient, the anesthesiologist or anesthetist, the surgeon, the intraoperative
nurses, and the surgical technologists. The anesthesiologist or nurse
anesthetist administers the anesthetic physical status throughout the
surgery. The surgeon and assistants scrub and perform the surgery. The
individual in the scrub role, either a nurse or surgical technologist, provides
sterile instruments and supplies to the surgeon during the procedure. The
circulating nurse coordinates the care of the patient in the operating room.
Care provided by the circulating nurse includes assisting with patient
positioning, preparing the patient’s skin for surgery, managing surgical
specimens, and documenting intraoperative events.
THE PATIENT
As the patient enters the operating room,
he or she may feel relaxed and prepared, or fearful and highly stressed. These
feelings depend very much on the amount and timing of preoperative sedation and
the patient’s level of fear and anxiety. Fears about loss of control, the
unknown, pain, death, changes in body structure or function, and disruption of
lifestyle all may contribute to a generalized anxiety. These fears can increase
the amount of anesthetic needed, the level of postoperative pain, and overall
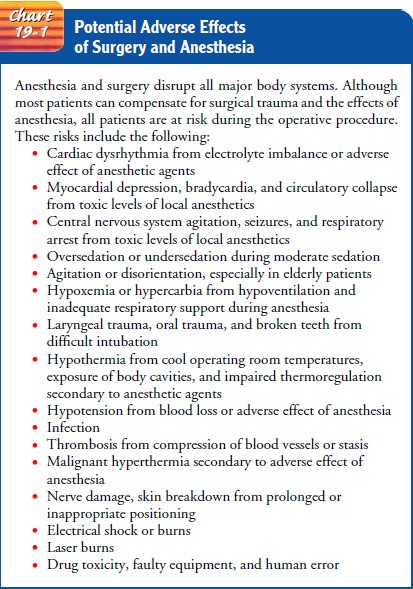
recovery time.The patient is also subject to several risks. Infection, failure
of the surgery to relieve symptoms, temporary or permanent complications
related to the procedure or the anesthetic, and deathare uncommon but potential
outcomes of the surgical experience (Chart 19-1). In addition to fears and
risks, the patient undergoing sedation and anesthesia temporarily loses both
cognitive func- tion and biologic self-protective mechanisms. Loss of pain
sense, reflexes, and ability to communicate subjects the intraoperative patient
to possible injury.
Gerontologic Considerations
Elderly patients face higher risks from
anesthesia and surgery than younger adult patients (Polanczyk et al., 2001).
Statistically,perioperative risk increases with each decade over 60 years,
often because of the increased incidence of coexisting disease. Modifications
tailored to the biologic changes of later life and the application of research
findings for this population can reduce the risks.
Biologic
variations of particular importance include age-related cardiovascular and
pulmonary changes (Townsend, 2002). The aging heart and blood vessels have
decreased ability to respond to stress. Reduced cardiac output and limited
cardiac reserve make the elderly patient vulnerable to changes in circulating
volume and blood oxygen levels. Excessive or rapid administration of
intravenous solutions may cause pulmonary edema. A sudden or prolonged drop in
blood pressure may lead to cerebral ischemia, thrombosis, embolism, infarction,
and anoxia. Reduced gas ex-change can lead to cerebral hypoxia.
The
elderly patient needs fewer anesthetics to produce anes-thesia and eliminates
the anesthetic agent over a longer time than a younger patient. As people age,
the percentage of lean body tis-sue decreases and fatty tissue steadily
increases (from age 20 years to 90 years). Anesthetic agents that have an
affinity for fatty tissue concentrate in body fat and the brain (Dudek, 2001).
Lower doses of anesthetic are appropriate for another reason. The older patient,
particularly when malnourished, may have low plasma protein lev-els. With
decreased plasma proteins, more of the anesthetic agent remains free or
unbound, and the result is more potent action.
Also
in elderly adults, body tissues made up predominantly of water and those with a
rich blood supply, such as skeletal muscle, liver, and kidneys, shrink. Reduced
liver size decreases the rate at which the liver can inactivate many
anesthetics, whereas de-creased kidney function slows elimination of waste products
and anesthetics. Other factors affecting the elderly surgical patient in the
intraoperative period include the following:
·
Impaired ability to increase
metabolic rate and impaired thermoregulatory mechanisms increase susceptibility
to hypothermia.
·
Bone loss (25% in women, 12% in men)
necessitates care-ful manipulation and positioning during surgery.
·
Reduced ability to adjust rapidly to
emotional and physical stress influences surgical outcomes and requires
meticulous observation of vital functions.
As
expected, mortality is higher with emergency surgery (com-monly required for
traumatic injuries) than with elective surgery, making continuous and careful
monitoring and prompt inter-vention especially important for older surgical
patients (Phippen & Wells, 2000).
Nursing Care
Throughout
surgery, nursing responsibilities include providing for the safety and
well-being of the patient, coordinating the op-erating room personnel, and
performing scrub and circulating activities. Because the patient’s emotional
state remains a con-cern, the care begun by preoperative nurses is continued by
the intraoperative nursing staff, who provide the patient with in-formation and
realistic reassurance. The nurse supports coping strategies and reinforces the
patient’s ability to influence out-comes by encouraging his or her active
participation in the plan of care.
In
the role of patient advocate, intraoperative nurses monitor factors that can
cause injury, such as patient position, equipment malfunction, and environmental
hazards, and they protect pa-tients’ dignity and interests while they are
anesthetized. Addi-tional responsibilities include maintaining surgical
standards of care, identifying existing patient risk factors, and assisting in
modifying complicating factors to help reduce operative risk (Phippen &
Wells, 2000).
THE CIRCULATING NURSE
The
circulating nurse (also known as the
circulator) must be a registered
nurse. He or she manages the operating room and protects the patient’s safety
and health by monitoring the ac-tivities of the surgical team, checking the
operating room con-ditions, and continually assessing the patient for signs of
injury and implementing appropriate interventions. The main re-sponsibilities
include verifying consent, coordinating the team, and ensuring cleanliness,
proper temperature, humidity, and lighting; the safe functioning of equipment;
and the availabil-ity of supplies and materials. The circulating nurse monitors
aseptic practices to avoid breaks in technique while coordinat-ing the movement
of related personnel (medical, radiography, and laboratory) as well as
implementing fire safety precautions (Phippen & Wells, 2000). The
circulating nurse monitors the patient and documents specific activities
throughout the oper-ation to ensure the patient’s safety and well-being.
Nursing ac-tivities directly relate to preventing complications and achieving
optimal patient outcomes.
THE SCRUB ROLE
Activities
of the scrub role include performing
a surgical hand scrub; setting up the sterile tables; preparing sutures,
ligatures, and special equipment (such as a laparoscope); and assisting the
surgeon and the surgical assistants during the procedure by anticipating the
instruments that will be required, such as sponges, drains, and other equipment
(Phippen & Wells, 2000). As the surgical incision is closed, the scrub
person and the cir-culator count all needles, sponges, and instruments to be
sure they are accounted for and not retained as a foreign body in the patient.
Tissue specimens obtained during surgery must also be labeled by the scrub
person and sent to the laboratory by the circulator.
THE SURGEON
The
surgeon performs the surgical procedure and heads the sur-gical team. He or she
is a licensed physician (MD), osteopath (DO), oral surgeon (DDS or DMD), or
podiatrist (DPM) who is specially trained and qualified. Qualifications may
include cer-tification by a specialty board, adherence to Joint Commission on
Accreditation of Healthcare Organizations ( JCAHO) standards, and adherence to
hospital standards and admitting practices and procedures (Fortunato, 2000).
THE REGISTERED NURSE FIRST ASSISTANT
The
registered nurse first assistant (RNFA) is another member of the operating room
staff. Although the scope of practice of the RNFA depends on each state’s nurse
practice act, the RNFA practices under the direct supervision of the surgeon.
RNFA re-sponsibilities may include handling tissue, providing exposure at the
operative field, suturing, and providing hemostasis. The en-tire process requires
a thorough understanding of anatomy and physiology, tissue handling, and the
principles of surgical asep-sis. The
competent RNFA needs to be aware of the objectives ofthe surgery, needs to have
the knowledge and ability to anticipate needs and to work as a skilled member
of a team, and needs to be able to handle any emergency situation in the
operating room (Fortunato, 2000; Rothrock, 1999).
THE ANESTHESIOLOGIST AND ANESTHETIST
An
anesthesiologist is a physician
specifically trained in the art and science of anesthesiology. An anesthetist is a qualified health care
professional who administers anesthetics. Most anesthetists are nurses who have
graduated from an accredited nurse anesthesia program and have passed
examinations sponsored by the American Association of Nurse Anesthetists to
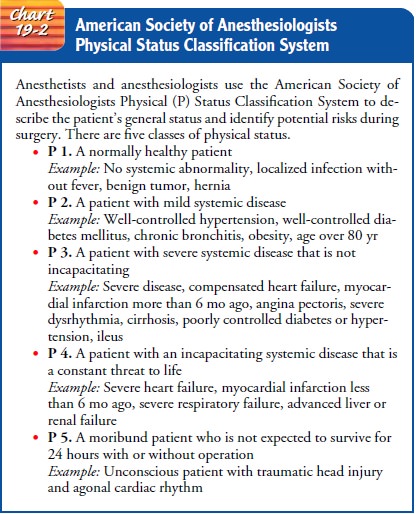
become a certified registered nurse anesthetist (CRNA). The anesthesiologist or
anesthetist in-terviews and assesses the patient prior to surgery, selects the
anes-thesia, administers it, intubates the patient if necessary, manages any
technical problems related to the administration of the anes-thetic agent, and
supervises the patient’s condition throughout the surgical procedure. Before
the patient enters the operating room, often at preadmission testing, the
anesthesiologist or anesthetist visits the patient to provide information and
answer questions. The type of anesthetic to be administered, previous reactions
to anes-thetics, and known anatomic abnormalities that would make air-way
management difficult are discussed. The anesthesiologist or anesthetist uses
the American Society of Anesthesiologists (ASA) Physical Status Classification
System to determine the patient’s status (Chart 19-2).
When the patient arrives in the operating room, the anesthe-siologist or anesthetist reassesses the patient’s physical condition immediately prior to initiating anesthesia. The anesthetic is ad-ministered, and the patient’s airway is maintained either through a laryngeal mask airway (LMA) or an endotracheal tube. During surgery, the anesthesiologist or anesthetist monitors the patient’s blood pressure, pulse, and respirations as well as the electrocar-diogram (ECG), blood oxygen saturation level, tidal volume, blood gas levels, blood pH, alveolar gas concentrations, and body temperature.
Monitoring by electroencephalography is some times
required. Levels of anesthetics in the body can also be de-termined; a mass
spectrometer can provide instant readouts of critical concentration levels on
display terminals. The device also assesses the patient’s ability to breathe
unassisted and indicates the need for mechanical assistance when ventilation is
poor and the patient is not breathing well independently.
Related Topics