Chapter: Medical Surgical Nursing: Intraoperative Nursing Management
Methods of Anesthesia Administration - Surgical Experience
METHODS OF ANESTHESIA ADMINISTRATION
Anesthetics
produce anesthesia because they are delivered to the brain at a high partial
pressure that enables them to cross the blood–brain barrier. Relatively large
amounts of anesthetic must be administered during induction and the early
maintenance phases because the anesthetic is recirculated and deposited in body
tissues. As these sites become saturated, smaller amounts of the anesthetic
agent are required to maintain anesthesia because equilibrium or near
equilibrium has been achieved between brain, blood, and other tissues.
Anything
that diminishes peripheral blood flow, such as vaso-constriction or shock, may
reduce the amount of anesthetic re-quired. Conversely, when peripheral blood
flow is unusually high, as in the muscularly active or the apprehensive
patient, induction is slower and greater quantities of anesthetic are re-quired
because the brain receives a smaller quantity of anesthetic.
Inhalation
Liquid
anesthetics may be administered by mixing the vapors with oxygen or nitrous
oxide–oxygen and then having the patient inhale the mixture (Townsend, 2002).
The vapor is administered to the patient through a tube or a mask. The
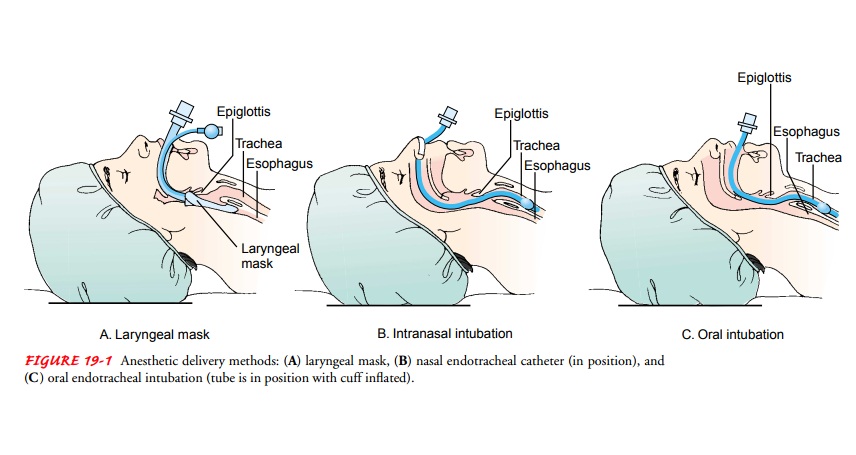
inhalation anesthetic may also be administered through a laryngeal mask (Fig.
19-1), a flexible tube with an inflatable silicone ring and cuff that can be
inserted into the larynx (Fortunato, 2000). The endotracheal technique for
administering anesthetics consists of introducing a soft rubber or plastic
endotracheal tube into the trachea, usually by means of a laryngoscope. The
endotracheal tube may be in-serted through either the nose or mouth. When in
place, the tube seals off the lungs from the esophagus so that if the patient
vom-its, stomach contents do not enter the lungs.
Intravenous
General
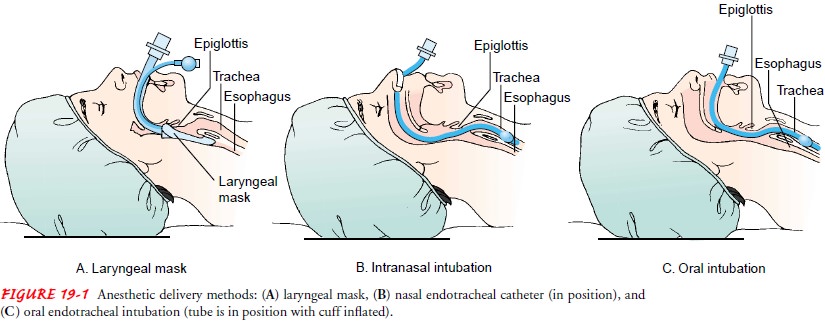
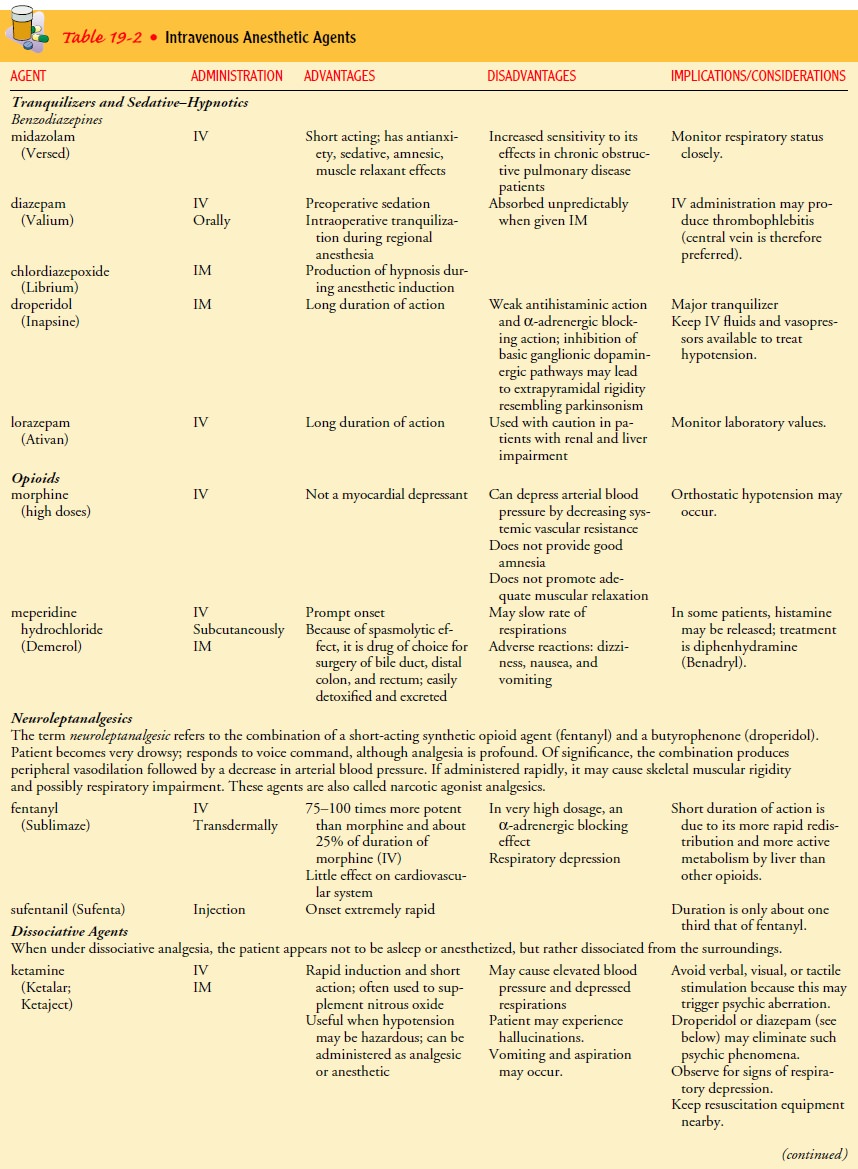
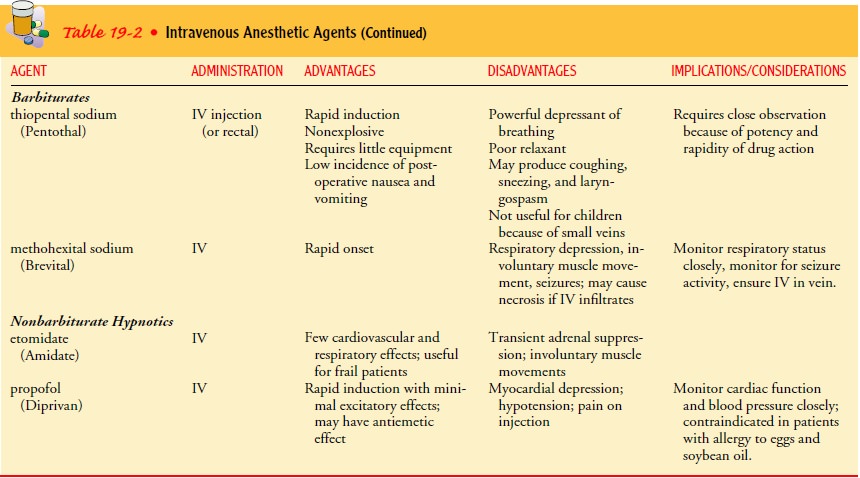
anesthesia can also be produced by the intravenous in-jection of various
substances, such as barbiturates, benzodiaze-pines, nonbarbiturate hypnotics,
dissociative agents, and opioid agents (Aranda & Hanson, 2000; Townsend,
2002). These med-ications may be administered for induction (initiation) or
main-tenance of anesthesia. They are often used along with inhalation
anesthetics but may be used alone. They can also be used to pro-duce moderate
sedation. Intravenous anesthetics are presented in Table 19-2.
An
advantage of intravenous anesthesia is that the onset of anesthesia is
pleasant; there is none of the buzzing, roaring, or dizziness known to follow
administration of an inhalation anesthetic. For this reason, induction of
anesthesia usually begins with an intravenous agent and is often preferred by
patients who have experienced various methods. The duration of action is brief,
and the patient awakens with little nausea or vomiting. Thiopental is usually
the agent of choice, and it is often administered with other anesthetic agents
in prolonged procedures.
Intravenous
anesthetic agents are nonexplosive, they require little equipment, and they are
easy to administer. The low inci-dence of postoperative nausea and vomiting
makes the method useful in eye surgery because vomiting would increase
intraocular pressure and endanger vision in the operated eye. Intravenous
anesthesia is useful for short procedures but is used less often for the longer
procedures of abdominal surgery. It is not indicated for children, who have
small veins and require intubation because of their susceptibility to
respiratory obstruction.
A
disadvantage of an intravenous anesthetic such as thiopen-tal is its powerful
respiratory depressant effect. It must be ad-ministered by a skilled
anesthesiologist or anesthetist and only when some method of oxygen
administration is available imme-diately in case of difficulty. Sneezing,
coughing, and laryngospasm are sometimes noted with its use.
Intravenous
neuromuscular blockers (muscle relaxants) block the transmission of nerve
impulses at the neuromuscular junction of skeletal muscles. Muscle relaxants
are used to relax muscles in abdominal and thoracic surgery, relax eye muscles
in certain types of eye surgery, facilitate endotracheal intubation, treat
laryngo-spasm, and assist in mechanical ventilation.
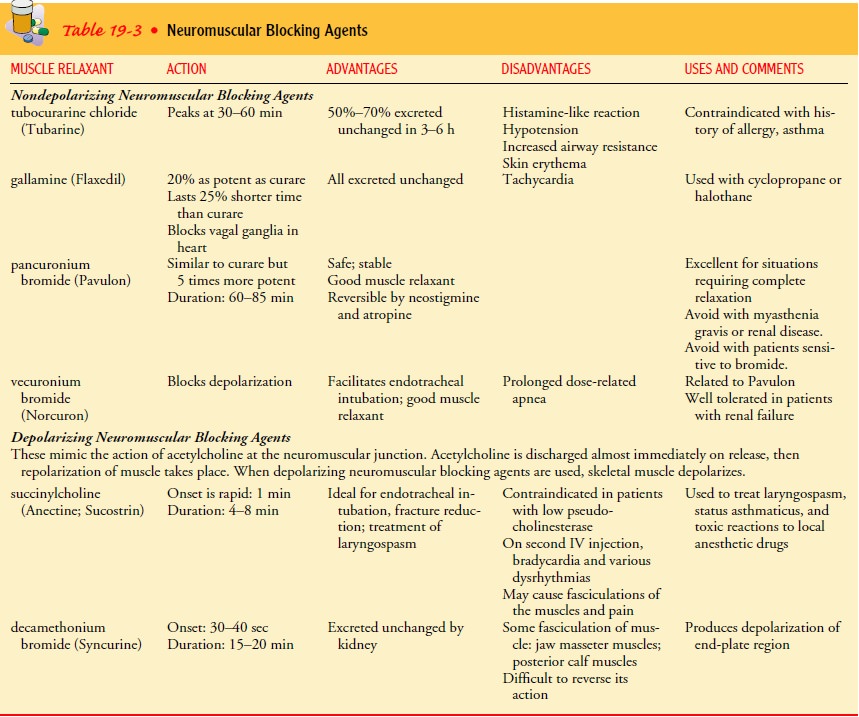
Purified
curare was the first widely used muscle relaxant; tubocu-rarine was isolated as
the active ingredient. Succinylcholine was later introduced because it acts
more rapidly than curare. Several other agents are also used (Table 19-3). The
ideal muscle relax-ant has the following characteristics:
·
It is nondepolarizing
(noncompetitive agent), with an onset and duration of action similar to
succinylcholine but with-out its problems of bradycardia and cardiac
dysrhythmias (Townsend, 2002).
·
It has a duration of action between
those of succinylcholine and pancuronium.
·
It lacks cumulative and cardiovascular
effects.
· It can be metabolized and does not depend on the kidneys for its elimination.
Regional Anesthesia
Regional
anesthesia is a form of local anesthesia in which an anes-thetic agent is
injected around nerves so that the area supplied by these nerves is
anesthetized. The effect depends on the type of nerve involved. Motor fibers
are the largest fibers and have the thickest myelin sheath. Sympathetic fibers
are the smallest and have a minimal covering. Sensory fibers are intermediate.
Thus, a local anesthetic blocks motor nerves least readily and sympa-thetic
nerves most readily. An anesthetic cannot be regarded as having worn off until
all three systems (motor, sensory, and au-tonomic) are no longer affected.
The
patient receiving spinal or local anesthesia is awake and aware of his or her
surroundings unless medications are given to produce mild sedation or to
relieve anxiety. The nurse must avoid careless conversation, unnecessary noise,
and unpleasant odors; these may be noticed by the patient in the OR and may
con-tribute to a negative view of the surgical experience. A quiet en-vironment
is therapeutic. The diagnosis must not be stated aloud if the patient is not to
know it at this time.
Conduction Blocks and Spinal Anesthesia
There
are many types of conduction blocks, depending on the nerve groups affected by
the injection. Epidural anesthesia is achieved by injecting a local anesthetic
into the spinal canal in the space surrounding the dura mater (Fig. 19-2).
Epidural anesthe-sia also blocks sensory, motor, and autonomic functions, but
it is differentiated from spinal anesthesia by the injection site and the
amount of anesthetic used. Epidural doses are much higher be-cause the epidural
anesthetic does not make direct contact with the cord or nerve roots.
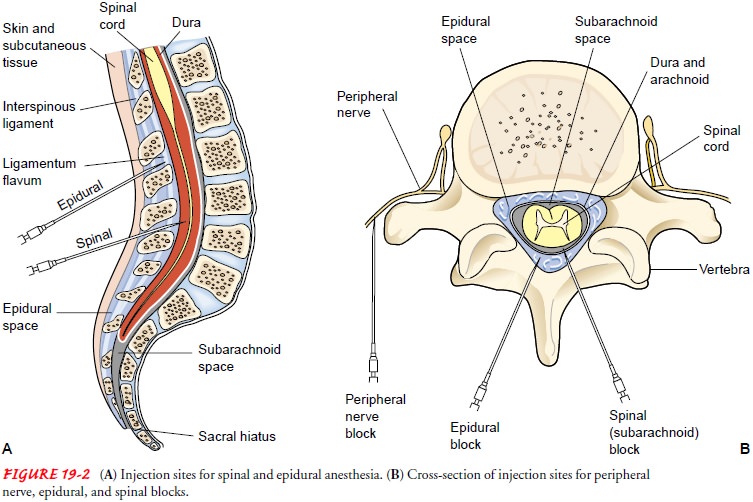
An
advantage of epidural anesthesia is the absence of headache that occasionally
results from subarachnoid injection. A disadvantage is the greater technical challenge of
introducing the anesthetic into the epidural rather than the subarachnoid
space. If inadvertent subarachnoid injection occurs during epidural anesthesia
and the anesthetic travels toward the head, high spinal anesthesia can result;
this can produce severe hypotension and respiratory depression and arrest.
Treatment of these compli-cations includes airway support, intravenous fluids,
and use of vasopressors. Other types of nerve blocks include:
·
Brachial plexus block, which
produces anesthesia of the arm
·
Paravertebral anesthesia, which
produces anesthesia of the nerves supplying the chest, abdominal wall, and
extremities
·
Transsacral (caudal) block, which
produces anesthesia of the perineum and, occasionally, the lower abdomen
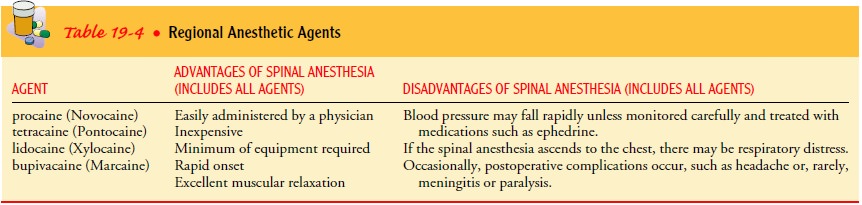
Spinal anesthesia is a type of extensive
conduction nerve block that is produced when a local anesthetic is introduced
into the subarachnoid space at the lumbar level, usually between L4 and L5 (see
Fig. 19-2). It produces anesthesia of the lower extremi-ties, perineum, and
lower abdomen. For the lumbar puncture procedure, the patient usually lies on
the side in a knee–chest po-sition. Sterile technique is used as a spinal
puncture is made and the medication is injected through the needle. As soon as
the in-jection has been made, the patient is positioned on his or her back. If
a relatively high level of block is sought, the head and shoulders are lowered.
The spread of the anesthetic agent and the level of anesthesia depend on the amount of fluid injected, the speed with which it is injected, the positioning of the patient after the injection, and the specific gravity of the agent. If the specific gravity is greater than that of cerebrospinal fluid (CSF), the agent moves to the de-pendent position of the subarachnoid space. If the specific grav-ity is less than that of CSF, the anesthetic moves away from the dependent position. The anesthesiologist or anesthetist controls the spread of the agent. Generally, the agents used are procaine, tetracaine (Pontocaine), lidocaine (Xylocaine), and bupivacaine (Marcaine) (Table 19-4).
A
few minutes after induction of a spinal anesthetic, anes-thesia and paralysis
affect the toes and perineum and then grad-ually the legs and abdomen. If the
anesthetic reaches the upper thoracic and cervical spinal cord in high
concentrations, a tem-porary partial or complete respiratory paralysis results.
Paralysis of the respiratory muscles is managed by mechanical ventilation until
the effects of the anesthetic on the respiratory nerves have worn off.
Nausea,
vomiting, and pain may occur during surgery when spinal anesthesia is used. As
a rule, these reactions result from ma-nipulation of various structures,
particularly those within the ab-dominal cavity. The simultaneous intravenous
administration of a weak solution of thiopental and inhalation of nitrous oxide
may prevent such reactions.
Headache may be an after-effect of
spinal anesthesia. Several factors are involved in the incidence of headache:
the size of the spinal needle used, the leakage of fluid from the subarachnoid
space through the puncture site, and the patient’s hydration sta-tus. Measures
that increase cerebrospinal pressure are helpful in relieving headache. These
include keeping the patient lying flat, quiet, and well hydrated.
In
continuous spinal anesthesia, the tip of a plastic catheter re-mains in the
subarachnoid space during the surgical procedure so that more anesthetics may
be injected as needed. This technique al-lows greater control of the dosage,
but there is greater potential for postanesthetic headache because of the
large-gauge needle used.
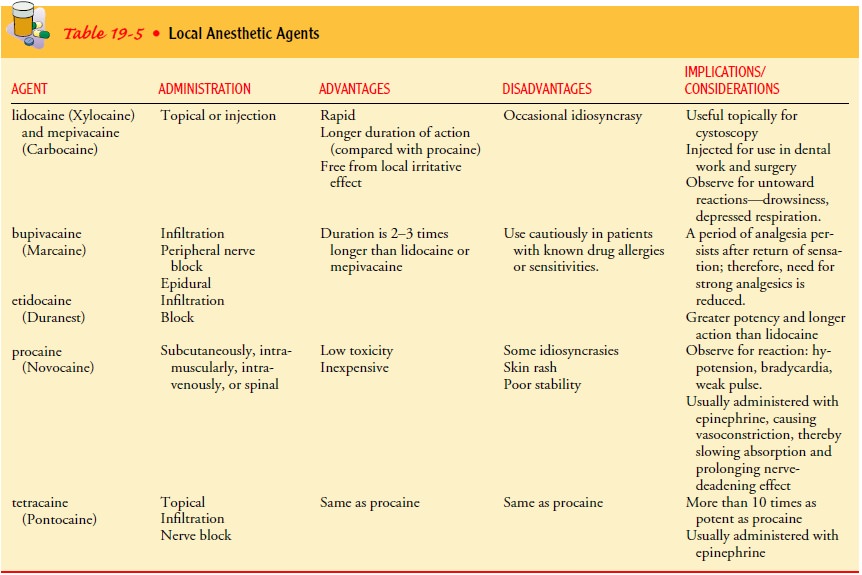
Local Infiltration Anesthesia
Infiltration
anesthesia is the injection of a solution containing the local anesthetic into
the tissues at the planned incision site. Often it is combined with a local
regional block by injecting the nerves immediately supplying the area. The
advantages of local anesthe-sia are as follows:
·
It is simple, economical, and
nonexplosive.
·
Equipment needed is minimal.
·
Postoperative recovery is brief.
·
Undesirable effects of general
anesthesia are avoided.
·
It is ideal for short and
superficial surgical procedures.
Local
anesthesia is often administered in combination with epinephrine. Epinephrine
constricts blood vessels, which pre-vents rapid absorption of the anesthetic
agent and thus prolongs its local action. Rapid absorption of the anesthetic
agent into the bloodstream, which could cause seizures, is also prevented.
Types of local anesthetic agents are listed in Table 19-5.
Local
anesthesia is the anesthesia of choice in any surgical pro-cedure in which it
can be used. However, contraindications in-clude high preoperative levels of
anxiety, because surgery with local anesthesia may increase anxiety. A patient
who requests gen-eral anesthesia rarely does well under local anesthesia. For
some surgical procedures, local anesthesia is impractical because of the number
of injections and the amount of anesthetic that would be required (breast
reconstruction, for example).
The
skin is prepared as for any surgical procedure, and a small-gauge needle is
used to inject a modest amount of the anesthetic into the skin layers. This
produces blanching or a wheal. Addi-tional anesthetic is then injected in the
skin until an area the length of the proposed incision is anesthetized. A
larger, longer needle then is used to infiltrate deeper tissues with the
anesthetic.The action of the agent is almost immediate, so surgery may begin as
soon as the injection is complete. Anesthesia lasts 45 minutes to 3 hours,
depending on the anesthetic and the use of epinephrine.
Related Topics