Chapter: Medical Surgical Nursing: Intraoperative Nursing Management
Sedation and Anesthesia - Surgical Experience
The Surgical Experience
During
the surgical procedure, the patient will need sedation, anesthesia, or a
combination of these.
SEDATION AND ANESTHESIA
Sedation
and anesthesia have four levels: minimal sedation, mod-erate sedation, deep
sedation, and anesthesia. Standards of care for each level have been set by
JCAHO. A surgical procedure may also be performed using anesthetic agents that
suspend sensation in parts of the body (local, regional, epidural, or spinal
anesthesia).
For
the patient, the anesthesia experience consists of having an intravenous line
inserted, if it was not inserted earlier; receiving a sedating agent prior to
induction with an anesthetic agent; losing consciousness; being intubated, if
indicated; and then receiving a combination of anesthetic agents. Typically the
experience is a smooth one and the patient has no recall of the events.
Minimal Sedation
The
minimal sedation level is a drug-induced state during which the patient can
respond normally to verbal commands. Cognitive function and coordination may be
impaired, but ventilatory and cardiovascular functions are not affected (JCAHO,
2001; Patter-son, 2000a, b).
Moderate Sedation
Moderate sedation is
a form of anesthesia that may be producedintravenously. It is defined as a
depressed level of consciousness that does not impair the patient’s ability to
maintain a patent air-way and to respond appropriately to physical stimulation
and ver-bal command. Its goal is a calm, tranquil, amnesic patient who, when
sedation is combined with analgesic agents, is relatively pain-free during the
procedure but able to maintain protective re-flexes (JCAHO, 2001; Patterson,
2000a, b). Sedation can be ad-ministered by an anesthesiologist, anesthetist,
other physician, or nurse. When administered by an anesthesiologist or
anesthetist, moderate sedation is referred to as monitored anesthesia care. The
medications permitted for use in moderate sedation vary with the credentials of
the person administering the sedative. In addition, state departments of health
are very specific about who may ad-minister moderate sedation and about the
training required for those individuals. These regulations vary greatly from
state to state.
Midazolam
(Versed) or diazepam (Valium) is used frequently for intravenous sedation. In
some states, the physician must ad-minister the first dose; a nurse with
special training can admin-ister subsequent doses. Other medications used
include analgesic agents (eg, morphine, fentanyl) and reversal agonists, such
as naloxone (Narcan). A nurse who is knowledgeable and skilled in detecting
dysrhythmias, administering oxygen, and performing resuscitation must
continuously monitor the patient who re-ceives sedation. The patient receiving
this form of anesthesia is never left alone and is closely monitored for
respiratory, cardio-vascular, and central nervous system depression using such
methods as pulse oximetry, ECG, and frequent measurement of vital signs
(Patterson, 2000a, b). The level of sedation is moni-tored by the patient’s
ability to maintain a patent airway and to respond to verbal commands.
Moderate
sedation may be used alone or in combination with local, regional, or spinal
anesthesia. Its use is increasing as more surgical procedures and diagnostic
studies are performed in ambulatory and same-day settings with the expectation
that the pa-tient will be discharged home a few hours after the procedure.
Deep Sedation
Deep
sedation is a drug-induced state during which a patient can-not be easily
aroused but can respond purposefully after repeated stimulation (JCAHO, 2001).
The difference between deep seda-tion and anesthesia is that the anesthetized
patient is not arousable. Deep sedation and anesthesia are achieved when an
anesthetic agent is inhaled or administered intravenously. Inhaled anesthetic
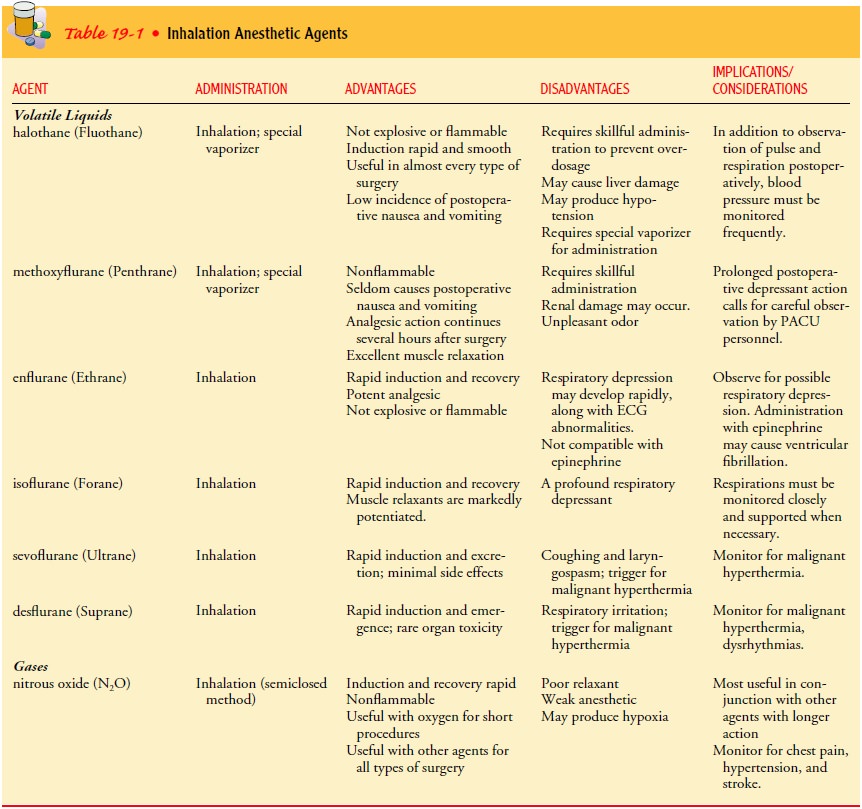
agents include volatile liquid agents and gases (Aranda & Hanson, 2000;
Townsend, 2002). Volatile liquid anesthetics produce anes-thesia when their
vapors are inhaled. Included in this group are halothane (Fluothane), enflurane
(Ethrane), isoflurane (Forane), sevoflurane (Ultrane), and desflurane
(Suprane). All are adminis-tered with oxygen, and usually with nitrous oxide as
well.
Gas
anesthetics are administered by inhalation and are always combined with oxygen.
Nitrous oxide is the most commonly used gas anesthetic. When inhaled, the
anesthetics enter the blood through the pulmonary capillaries and act on
cerebral centers to produce loss of consciousness and sensation. When
anesthetic ad-ministration is discontinued, the vapor or gas is eliminated
through the lungs. Table 19-1 lists the advantages, disadvantages, and
im-plications of the different volatile liquid and gas anesthetics.
Anesthesia
General
anesthesia consists of four stages, each associated with specific clinical
manifestations. When opioid agents (narcotics) and neuromuscular blockers
(relaxants) are administered, several of the stages are absent. The anesthesia
level consists of general anesthesia and spinal or major regional anesthesia
but does not include local anesthesia ( JCAHO, 2001). Anesthesia is a state of narcosis (severe central nervous system
depression produced by pharmacologic agents), analgesia, relaxation, and reflex
loss. Pa-tients under general anesthesia are not arousable, even to painful
stimuli. They lose the ability to maintain ventilatory function and require
assistance in maintaining a patent airway. Cardiovascular function may be
impaired as well (JCAHO, 2001).
STAGE I: BEGINNING ANESTHESIA
As
the patient breathes in the anesthetic mixture, warmth, dizzi-ness, and a
feeling of detachment may be experienced. The patient may have a ringing,
roaring, or buzzing in the ears and, though still conscious, may sense an
inability to move the extremities easily. During this stage, noises are exaggerated;
even low voices or minor sounds seem loud and unreal. For this reason, the
nurse avoids making unnecessary noises or motions when anesthesia begins.
STAGE II: EXCITEMENT
The
excitement stage, characterized variously by struggling, shouting, talking,
singing, laughing, or crying, is often avoided if the anesthetic is
administered smoothly and quickly. The pupils dilate, but contract if exposed
to light; the pulse rate is rapid, and respirations may be irregular.
Because of the possibility of uncontrolled movements of the patient during this stage, the anesthesiologist or anesthetist must always be assisted by someone ready to help restrain the patient. A strap may be in place across the patient’s thighs, and the hands may be secured to an armboard. The patient should not be touched except for purposes of restraint, but restraints should not be ap-plied over the operative site. Manipulation increases circulation to the operative site and thereby increases the potential for bleeding.
STAGE III: SURGICAL ANESTHESIA
Surgical
anesthesia is reached by continued administration of the anesthetic vapor or
gas. The patient is unconscious and lies quietly on the table. The pupils are
small but contract when ex-posed to light. Respirations are regular, the pulse
rate and volume are normal, and the skin is pink or slightly flushed. With
proper administration of the anesthetic, this stage may be maintained for hours
in one of several planes, ranging from light (1) to deep (4), depending on the
depth of anesthesia needed.
STAGE IV: MEDULLARY DEPRESSION
This
stage is reached when too much anesthesia has been admin-istered. Respirations
become shallow, the pulse is weak and thready, and the pupils become widely
dilated and no longer con-tract when exposed to light. Cyanosis develops and,
without prompt intervention, death rapidly follows. If this stage devel-ops,
the anesthetic is discontinued immediately and respiratory and circulatory
support is initiated to prevent death. Stimulants,although rarely used, may be
administered; narcotic antagonists can be used if overdosage is due to opioids.
During
smooth administration of an anesthetic, there is no sharp division between the
first three stages, and there is no stage IV. The patient passes gradually from
one stage to another, and it is only by close observation of the signs
exhibited by the patient that an anesthesiologist or anesthetist can control
the situation. The re-sponses of the pupils, the blood pressure, and the
respiratory and cardiac rates are probably the most reliable guides to the
patient’s condition.
Related Topics