Chapter: Medical Surgical Nursing: Health Education and Health Promotion
The Nursing Process in Patient Teaching
The Nursing Process in Patient Teaching
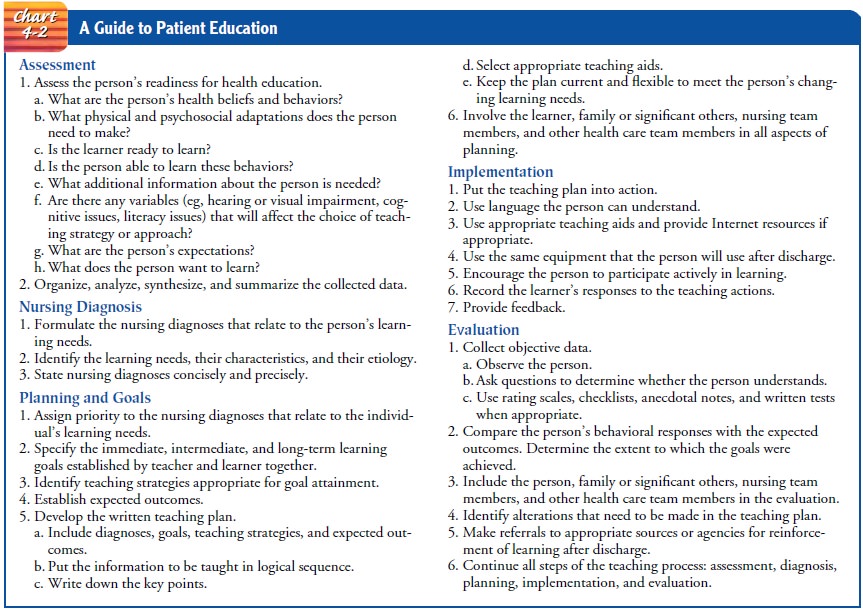
The steps of the nursing
process—assessment, diagnosis, plan-ning, implementation, and evaluation—are
used when con-structing a teaching plan to meet an individual’s teaching and
learning needs (Chart 4-2).
ASSESSMENT
Assessment in the
teaching–learning process is directed toward the systematic collection of data
about the person’s learning needs, the person’s readiness to learn, and the
family’s learning needs. All in-ternal and external variables that affect the
patient’s readiness to learn are identified. A learning assessment guide may be
used for this purpose. Some of the available guides are very general and are
directed toward the collection of general health information, whereas others
are specific to common medication regimens or disease processes. Such guides facilitate
the assessment but must be adapted to the individual’s responses, problems, and
needs.
As soon as possible
after completing the assessment, the nurse organizes, analyzes, synthesizes,
and summarizes the data col-lected and determines the patient’s need for
teaching.
NURSING DIAGNOSIS
Formulating nursing
diagnoses makes educational goals and eval-uations of progress more specific
and meaningful. Teaching is an integral intervention implied by all nursing
diagnoses, and for some diagnoses education is the primary intervention.
Ineffective therapeutic regimen management, Impaired home maintenance,
Health-seeking behaviors, and Decisional conflict are examples of nursing
diagnoses that direct planning for educational needs. The diagnosis “Deficient
knowledge” should be used cautiously, because knowledge deficit is not a human
response but a factor relating to or causing the diagnosis (eg, Ineffective
therapeutic regimen management related to a deficiency of information about
wound care is a more appropriate nursing diagnosis than “Defi-cient knowledge”)
(Carpenito, 1999). A nursing diagnosis that relates specifically to the
patient’s and family’s learning needs will serve as a guide in the development
of the teaching plan.
PLANNING
Once the nursing diagnoses
have been identified, the planning component of the teaching–learning process
is established in ac-cordance with the steps of the nursing process:
·Assigning priorities to
the diagnoses
·Specifying the
immediate, intermediate, and long-term goals of learning
·Identifying specific teaching strategies appropriate for at-taining goals
·
Specifying the expected outcomes
·
Documenting the diagnoses, goals, teaching
strategies, and expected outcomes on the teaching plan
As in the nursing
process, the assignment of priorities to the diagnoses should be a joint effort
by the nurse and the learner or family members. Consideration must be given to
the urgency of the individual’s learning needs, with the most critical needs
re-ceiving the highest priority.
After the priorities of
the diagnoses have been established, the immediate and long-term goals and the
teaching strategies ap-propriate for attaining the goals are identified.
Teaching is most effective when the objectives of both the learner and the
nurse are in agreement (Lorig, et al., 1996). Learning begins with the
es-tablishment of goals that are appropriate to the situation and re-alistic in
terms of the individual’s ability and desire to achieve them. Involving the
patient and family in establishing goals and subsequently in the planning of
teaching strategies promotes their cooperation in the implementation of the
teaching plan.
Expected outcomes of
teaching strategies can be stated in terms of behaviors of the person, the
family, or both. Outcomes should be realistic and measurable, and the critical
time periods for attaining them should also be identified. The desired
out-comes and the critical time periods will serve as a basis for evalu-ating
the effectiveness of the teaching strategies.
During the planning
phase, the nurse must consider the se-quence in which the subject matter will
be presented in each of the teaching strategies. Critical information (eg,
survival skills for the person with diabetes) and material that the person or
family identifies to be of particular importance receive high priority. An
outline is often helpful for arranging the subject matter and for ensuring that
all necessary information is included. Also during this time, appropriate
teaching aids to be used in implementing the teaching strategies are prepared
or selected.
The entire planning
phase of the teaching–learning process is concluded with the formulation of the
teaching plan. This teach-ing plan communicates the following information to
all members of the nursing team:
1) The nursing diagnoses
that specifically relate to the indi-vidual’s learning needs and the priorities
of these diagnoses
2) The goals of the
teaching strategies
3) The teaching strategies,
expressed in the form of teaching orders
4) The expected outcomes,
which identify the desired behav-ioral responses of the learner
5) The critical time period
within which each outcome is expected to be met
6) The individual’s
behavioral responses (which must be doc-umented on the teaching plan)
The same rules that apply to writing and
revising the plan of nursing care apply to the teaching plan.
IMPLEMENTATION
In the implementation
phase of the teaching–learning process, the patient, the family, and other
members of the nursing and health care teams carry out the activities outlined
in the teaching plan. The nurse coordinates all the activities.
Flexibility during the
implementation phase of the teaching– learning process and ongoing assessment
of the individual’s re-sponses to the teaching strategies support modification
of the teaching plan as necessary. Creativity in promoting and sustain-ing the
learner’s motivation to learn is essential. New learning needs that may arise
after discharge from the hospital or after home care visits have ended should
also be taken into account.
The implementation phase
is concluded when the teaching strategies have been completed and when the
individual’s re-sponses to the actions have been recorded. This record serves
as the basis for evaluating how well the defined goals and expected outcomes
have been achieved.
EVALUATION
Evaluation of the
teaching–learning process determines how ef-fectively the person has responded
to the teaching strategies and to what extent the goals have been achieved. An
important part of the evaluation phase addresses the question, “What can be
done to improve the teaching and enhance the learning?” An-swers to this
question will direct the changes to be made in the teaching plan.
An evaluation must be
made of what was done well, and what needs to be changed or reinforced. It
cannot be assumed that indi-viduals have learned just because teaching has
occurred: learning does not automatically follow teaching. A variety of
measurement techniques can be used to identify changes in behavior as evidence
that learning has taken place. These techniques include directly ob-serving the
behavior; using rating scales, checklists, or anecdotal notes to document the
behavior; and indirectly measuring results through oral questioning and written
tests. Measurement of actual behavior (direct measurement) is the most accurate
and appropri-ate technique in many patient teaching situations. Nurses often do
comparative analysis using patient admission data as the baseline: selected
data points observed during the period when nursing care is given and self-care
was initiated are compared with the patient’s baseline data.
Some examples of
indirect measurements are patient satisfac-tion surveys, attitude surveys, and
instruments that evaluate spe-cific health status variables. All direct
measurements should be supplemented with indirect measurements whenever
possible. Using more than one measuring technique enhances the reliabil-ity of
the resulting data and decreases the potential for error from a specific
measurement strategy.
Measuring is only the
beginning of evaluation. It must be fol-lowed by interpreting the data and
making value judgments about the learning and teaching. Such evaluation should
be conducted periodically throughout the teaching–learning program, at its
con-clusion, and at varying periods after the teaching has ended.
Evaluation of learning
after hospitalization is highly desir-able, because the analysis of teaching
outcomes must extend into home care. With shortened lengths of hospital stay
and with short-stay and same-day surgical procedures, follow-up evaluation in
the home is especially important. Coordination of efforts and sharing of
information between hospital-based and community-based nursing personnel
facilitates post-discharge teaching and home care evaluation.
Evaluation is not the
end step in the teaching–learning process, but the beginning of a new patient
assessment. The information gathered during evaluation should be used to
redirect teaching ac-tions, with the goal of improving the learner’s responses
and out-comes.
Related Topics