Chapter: Medical Surgical Nursing: Health Education and Health Promotion
Health Promotion
Health Promotion
Health teaching and
health promotion are linked by a common goal—to encourage people to achieve as
high a level of wellness as possible so that they can live maximally healthy
lives and avoid preventable illnesses. The call for health promotion has become
a cornerstone in health policy because of the need to control costs and reduce
unnecessary sickness and death.
The nation’s first
public health agenda was established in 1979 and set goals for improving the
health of all Americans. Addi-tional goals defined as the “1990 Health
Objectives” identified improvements to be made in health status, risk
reduction, public awareness, health services, and protective measures (U.S.
Public Health Service, 1990).
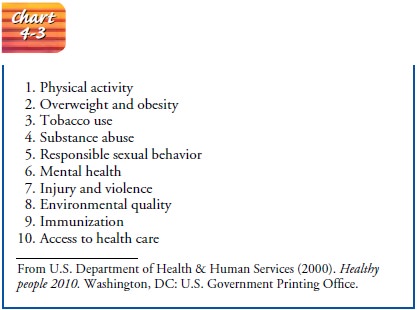
Health goals for the
nation were also established in the publi-cation, Healthy People 2000. The priorities from this initiative were
identified as health promotion, health protection, and the use of preventive
services. The most recent publication, HealthyPeople
2010, defines the current national health promotion anddisease prevention
initiative for the nation. The two essential goals from this report are (1) to
increase the quality and years of healthy life for people, and (2) to eliminate
health disparities among various segments of the population (U.S. Public Health
Service, 2000) (Chart 4-3).
HEALTH AND WELLNESS
The concept of health
promotion has evolved because of a chang-ing definition of health and an
awareness that wellness exists at many levels of functioning. The definition of
health as the mere absence of disease is no longer accepted. Today, health is
viewed as a dynamic, ever-changing condition that enables a person to function
at an optimum potential at any given time. The ideal health status is one in
which people are successful in achieving their full potential regardless of any
limitations they might have.
Wellness, as a
reflection of health, involves a conscious and de-liberate attempt to maximize
one’s health. Wellness does not just happen; it requires planning and conscious
commitment and is the result of adopting lifestyle behaviors for the purpose of
at-taining one’s highest potential for well-being. Wellness is not the same for
every person. The person with a chronic illness or dis-ability may still be
able to achieve a desirable level of wellness. The key to wellness is to
function at the highest potential within the limitations over which there is no
control.
A significant amount of information has shown that people, by virtue of what they do or fail to do, influence their own health. Today, many of the major causes of illness are chronic diseases that have been closely related to lifestyle behaviors (eg, heart disease, lung and colon cancer, chronic obstructive pulmonary diseases, hypertension, cirrhosis, traumatic injury, HIV [human immuno-deficiency virus] infection, and acquired immunodeficiency syn-drome [AIDS]). Consequently, a person’s health status to a large extent is reflective of lifestyle.
HEALTH PROMOTION MODELS
Since the 1950s, many
health-promotion models have been con-structed to identify health-protecting
behaviors and to help ex-plain what makes people engage in these preventive
behaviors. A health-protecting behavior is defined as any behavior performed by
people, regardless of their actual or perceived health condition, for the
purpose of promoting or maintaining their health, whether or not the behavior
produces the desired outcome (Downie, Fyfe,
Tannahill, 1990). One framework, the health
belief model, was devised to foster understanding of what made some healthy
people choose actions to prevent illness while others refused to engage in
these protective recommendations (Becker, 1974).
Another model, the
resource model of preventive health be-havior (Downie, Fyfe, & Tannahill,
1990), addresses the ways that people use resources to promote health. Nurse
educators can use this model to assess how demographic variables, health
be-haviors, and social and health resources influence health promo-tion.
LaLonde’s (1977) health determinants model views human biology, environment,
lifestyle, and the health care delivery sys-tem as the four determinants of a
person’s health.
A model for promotion of
health, designed by Becker and colleagues (1993), is based on the premise that
four variables in-fluence the selection and use of health promotion behaviors.
The first variable, demographic and disease factors, includes client
characteristics such as age, gender, education, employment, sever-ity of
illness or disability, and length of illness. Barriers, the next component, are
defined as factors that lead to unavailability or difficulty in gaining access
to a specific health promotion alter-native. The third variable, resources,
encompasses such items as financial and social support. The last variable,
perceptual factors, consists of how people view their health status,
self-efficacy, and the perceived demands of their illness. The developers of
this model conducted research to substantiate that these four vari-ables have a
positive correlation with a person’s quality of life.
The health promotion
model developed by Pender (1996), is based on social learning theory and
emphasizes the importance of motivational factors that influence the acquiring
and sustain-ing of health-promotion behaviors. This model explores how
cognitive-perceptual factors affect one’s view of the importance of health. It
also examines perceived control of health, self-efficacy, health status, and the
benefits and barriers to health promoting behaviors.
These models, along with
other examples that can be found in the health promotion literature, can serve
as an organizing frame-work for clinical work and research that supports the
enhance-ment of health. Further efforts, however, are needed to advance
understanding of the health promotion behaviors of families and communities.
DEFINITION OF HEALTH PROMOTION
Health promotion can be
defined as those activities that assist in-dividuals in developing resources
that will maintain or enhance well-being and improve their quality of life.
These activities in-volve a person’s efforts to remain healthy in the absence
of symp-toms and do not require the assistance of a health care team member.
The purpose of health
promotion is to focus on a person’s po-tential for wellness and to encourage
appropriate alterations in personal habits, lifestyle, and environment in ways
that will re-duce risks and enhance health and well-being. Health promotion is
an active process; that is, it is not something that can be pre-scribed or
dictated. It is up to the individual to decide whether to make the changes that
will promote a higher level of wellness. Choices must be made, and only the
individual can make these choices.
The concepts of health,
wellness, health promotion, and dis-ease prevention have been extensively
addressed in the lay litera-ture and news media as well as in professional
journals. The result has been a public demand for health information and a
response by health care professionals and agencies to provide this
infor-mation. Health-promotion programs that were once limited to hospital
settings have now moved into community settings such as clinics, schools,
churches, businesses, and industry. The work-place is quickly becoming an
important site for health promotion programs, as employers strive to reduce
costs associated with ab-senteeism, health insurance, hospitalization,
disability, excessive turnover of personnel, and premature death.
HEALTH PROMOTION PRINCIPLES
Certain principles
underlie the concept of health promotion as an active process:
self-responsibility, nutritional awareness, stress reduction and management,
and physical fitness.
Self-Responsibility
Taking responsibility
for oneself is the key to successful health promotion. The concept of self-responsibility is based on the
understanding that individuals control their lives. Each of us alone must make
those choices that determine how healthy our lifestyle is. As more people
recognize the significant effects that lifestyle and behavior have on health,
they may assume responsi-bility for avoiding high-risk behaviors such as
smoking, alcohol and drug abuse, overeating, driving while intoxicated, risky
sex-ual practices, and other unhealthy habits. They may also assume
responsibility for adopting routines that have been found to have a positive
influence on health, such as engaging in regular exer-cise, wearing a seat
belt, and eating a balanced diet.
A variety of different
techniques have been used to encourage people to accept responsibility for
their health, ranging from exten-sive educational programs to reward systems.
No one technique has been found to be superior to any other. Instead,
self-responsibility for health promotion is very individualized and depends on
a person’s desires and inner motivations. Health promotion pro-grams are
important tools for encouraging people to assume re-sponsibility for their
health and to develop behaviors that improve health.
Nutrition
Nutrition as a component of health promotion has become
thefocus of considerable attention and publicity. A vast array of books and
magazine articles address the topics of special diets, natural foods, and the
hazards of certain substances, such as sugar, salt, cholesterol, artificial
colors, and food additives. Good nutri-tion has been suggested as the single
most significant factor in determining health status and longevity.
Nutritional awareness
involves an understanding of the im-portance of a properly balanced diet that
supplies all of the essential nutrients. Understanding the relationship between
diet and disease is an important facet of a person’s self-care. Some clinicians
believe that a healthy diet is one that substitutes “nat-ural” foods for
processed and refined ones and reduces the intake of sugar, salt, fat,
cholesterol, caffeine, alcohol, food additives, and preservatives.
Stress Management
Stress management and stress reduction are important aspects
ofhealth promotion. Studies have shown the negative effects of stress on health
and a cause-and-effect relationship between stress and infectious diseases,
traumatic injuries (eg, motor vehicle crashes), and some chronic illnesses.
Stress has become inevitable in con-temporary societies in which demands for
productivity have be-come excessive. More and more emphasis is placed on
encouraging people to manage stress appropriately and to reduce stress that is
counterproductive. Techniques such as relaxation training, exer-cise, and
modification of stressful situations are often included in health promotion
programs that deal with stress. Further infor-mation on stress management,
including health risk appraisal and stress reduction methods such as
biofeedback and the relaxation response.
Exercise
Physical fitness is another important component of
healthpromotion. Clinicians and researchers (Anspaugh, Hamrick & Rosata,
1994; Edelman & Mandle, 1998; U.S. Department of Health & Human
Services, 1996) examining the relationship be-tween health and physical fitness
have found that a regular exer-cise program can promote health by improving the
function of the circulatory system and the lungs, decreasing cholesterol and
low-density lipoprotein concentrations, lowering body weight by increasing
calorie expenditure, delaying degenerative changes such as osteoporosis, and
improving flexibility and overall mus-cle strength and endurance. On the other
hand, exercise can be harmful if it is not started gradually and increased
slowly in ac-cordance with the individual’s response. An exercise program
should be designed specifically for the individual, with consider-ation given
to age, physical condition, and any known cardio-vascular or other risk
factors. An appropriate exercise program can have a significantly positive
effect on the individual’s perfor-mance capacity, appearance, and general state
of physical and emotional health (Nursing Research Profile 4-2).
Related Topics