Chapter: Essentials of Psychiatry: Psychiatric Epidemiology
The Epidemiological Catchment Area Study
The Epidemiological Catchment Area
Study
In response to the 1978 President’s Commission on
Mental Health Report, NIMH sponsored the Epidemiological Catch-ment Area (ECA)
project to determine the prevalence of mental disorders in specific sites and
the proportion receiving mental health services (Regier et al., 1984). Parallel to the planning of the ECA study, the APA
published the DSM-III (American Psychiatric Association, 1980), which had
clearly defined opera-tional criteria that facilitated case definition. Thus,
the concept of a case as a discrete entity that had been achieved in the late
1970s permitted the categorical determination of psychiatric caseness as
opposed to the dimensional assessment of symptomimpairment. As a prelude to the
ECA, the NIMH cosponsored the development of the Diagnostic Interview Schedule (reviewed
above).
The basic design involved face-to-face baseline
interviews with random samples of adults selected from the catchment ar-eas,
6-month telephone follow-up interviews to obtain interim information on medical
and psychiatric service use, and 1-year face-to-face interviews with the
original sample. The initial re-sponse rate ranged from 68% (Los Angeles) to
79% (St Louis and Durham) (Leaf et al.,
1991). Overall, 12% of the original re-spondents were lost to or refused to
participate in the follow-up interview. Eaton and collaborators (1992) reported
that failure to be tracked was associated with being male, young, unmarried and
Hispanic; refusal to participate was associated with being older, married and
uneducated
Prevalence
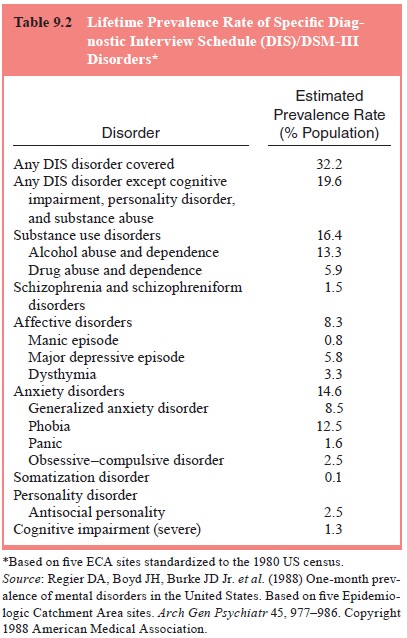
Overall, 32.2% of the adults included in the five
sites met crite-ria for one or more of the assessed mental disorders during
their lifetime (Table 9.2. Phobias and alcohol abuse and dependence were the
most common mental disorders (Regier et
al., 1985). The lifetime prevalence for phobia was 12.5%, and the 1-month
prevalence was 6.2%. The rates for drug abuse and dependence were 5.9% for
lifetime and 1.3% for 1-month prevalence.
The ECA study investigators did extensive analyses
of the variation in prevalence rates by demographic characteristics
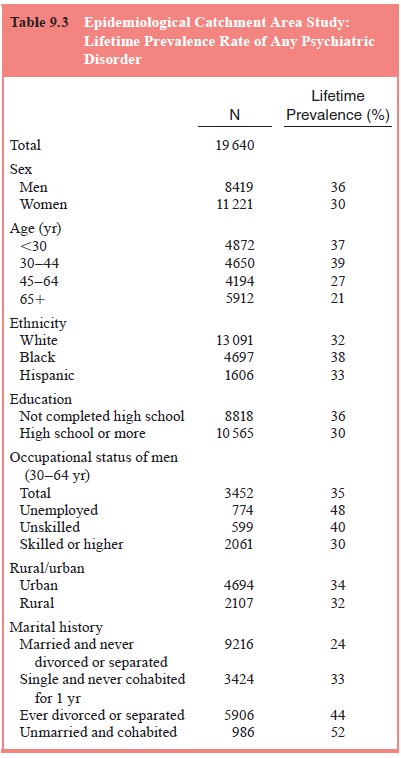
For lifetime diagnosis, 36% of men at some point
suffered from an addictive or mental disorder, compared with 30% of women
(Table 9.3).
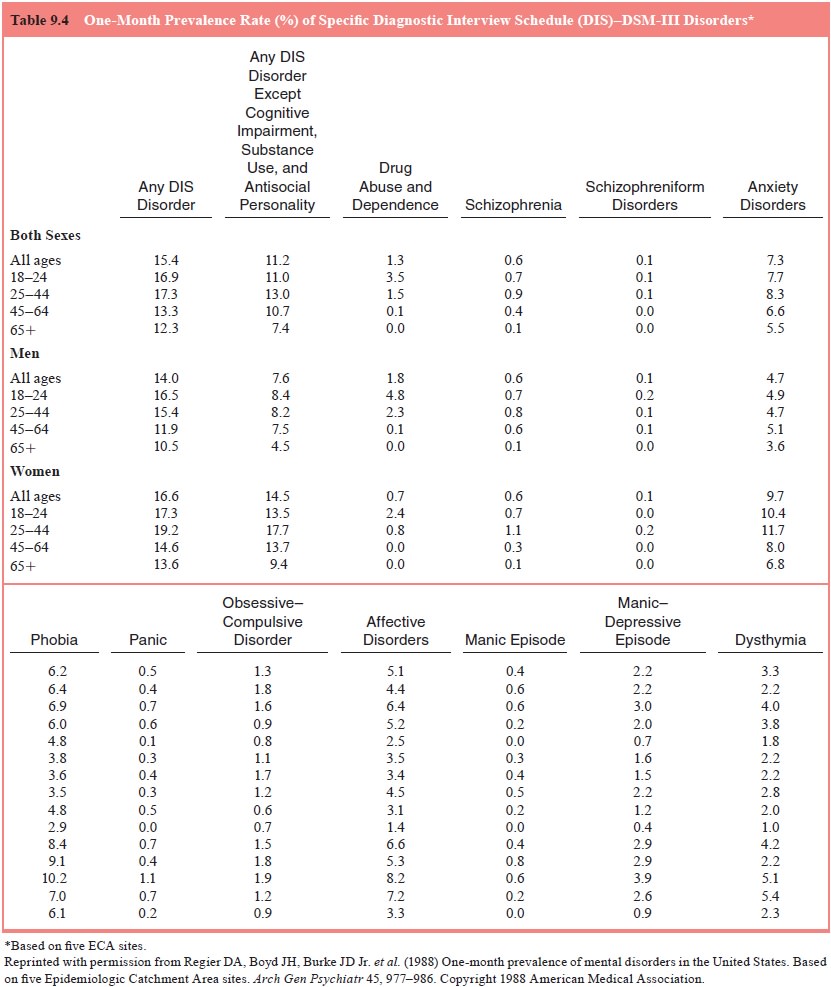
The pooled 1-month prevalence rates for the five
sites (see Table 9.4) was 15.4% for all ages for any DSM-III disorder. The age
group 25 to 44 years had the highest overall rate of 17.3%. Although this age
pattern was also true for women, men aged 18 to 24 years had the highest
overall rate. This occurred because of the peak in rates of drug abuse and
dependence in men in this age group. Anxiety disorders were most prevalent at
11.7% in women 25 to 44 years old, compared with only 4.7% for men in the same
group. The overall prevalence for all affective disorders was 5.1%; the age
group with the highest prevalence was women 25 to 44 years old.
Incidence
Incidence rates were calculated based on the
12-month follow-up assessments of healthy individuals found during the initial
as-sessments (Regier et al., 1993).
During the 1-year follow-up period, 6% of the total
popu-lation had one or more new disorders (Regier et al., 1993). Also, 5.7% of those with a history of a mental
disorder suffered a re-lapse or a new condition in the 1-year period for a
total of 12.3% of new cases in 1 year.
Use of Mental Health Services
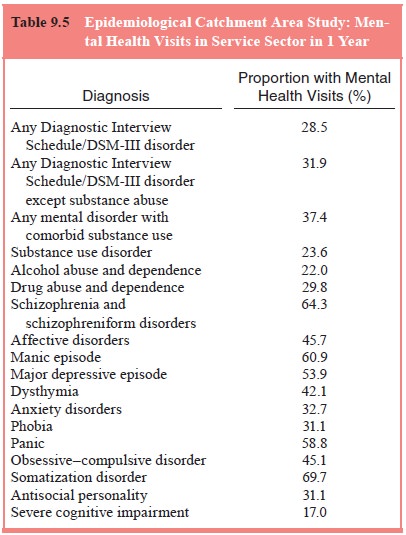
Although 28.1% of the sample had diagnosable mental
or addic-tive disorders, only 14.7% (23 million) received care, indicating that
a disproportionate number of individuals suffering from mental and addictive
disorders did not receive treatment. Con-versely, although 22% of respondents
who had recently used a medical care facility met criteria for a DSM-III
disorder, 17% of nonusers had a diagnosable illness (Regier et al., 1993; Eaton et al., 1992; Narrow et al.,
1993, Kessler et al., 1987). The
dis-orders making the greatest contribution were alcohol abuse and dependence
in men and major depression in women. The ECA study found that 0.9% received inpatient
treatment in a specialty mental and addictive disorders facility during a
1-year period. Among individuals with any DSM-III disorder who received mental
health services, 28.5% sought treatment from either a mental health clinician
or medical physician (see Table 9.5).
Comorbidity of Mental and Substance Use Disorders
The ECA study provided valuable data about the
prevalence of comorbidity of alcohol and substance use disorders with mental
disorders (Regier et al., 1985,
1990). Before the ECA study, most of the information about comorbidity came
from populations in treatment settings. Since the early 1950s, it has
repeatedly been found that patients in clinical settings typically present
them-selves for treatment because they have more than one disorder, a
phenomenon first described by Berkson (1946). Thus, clinical populations
provide a biased (and inflated) view of comorbidity.
The ECA study defined comorbidity as the occurrence
of more than one disorder and did not require that the disorders overlap
temporally. Up to 29% of individuals with a mental disor-der suffer from a
comorbid substance use disorder. Similarly, in-dividuals with alcohol use
disorder have twice the risk of having a comorbid mental disorder and more than
five times the risk of having a comorbid drug use disorder. Among individuals
with al-cohol use disorders, the most common comorbid mental disorder was
anxiety disorder, with a prevalence of 19.4%. For individuals with drug use
disorder, 22% suffered from a mental disorder.
In summary, findings from the ECA confirmed the
wide-spread and impairing nature of mental disorders reported in the
second-generation community studies described above. The methodologic rigor
with which the ECA was conducted was in-strumental at dispelling the disbelief
and criticism of methodo-logy that frequently accompanied second-generation
studies. The rates in the five ECA sites confirmed the high prevalence of
untreated mental disorder. ECA results, such as the finding that individuals
with mental disorders were relatively more likely to use general medical
services compared with those without disor-ders, raised provocative questions
for a new generation of psychi-atric epidemiologists.
Related Topics