Chapter: Obstetrics and Gynecology: Menopause
Symptoms and Signs of Menopause
SYMPTOMS AND SIGNS OF MENOPAUSE
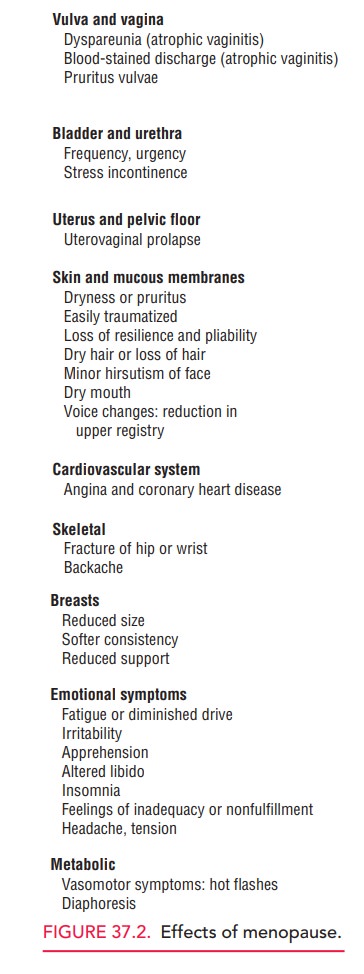
Menopause is a physiologic
process that can be associated with symptoms that may affect a woman’s quality
of life.
Decreased
estrogen production can result in multiple systemic effects (Fig. 37.2). Many
of these symptoms can be amelio-rated with hormone therapy. The need for
hormone therapy should be individualized based on a woman’s specific risk
factors.
Menstrual Cycle Alterations
Beginning at approximately 40
years of age, the number of a woman’s ovarian follicles diminishes, and subtle
changes occur in the frequency and length of menstrual cycles. A woman may note
shortening or lengthening of her cycles. The luteal phase of the cycle remains
constant at 13 to 14 days, whereas the variation of cycle length is related to
a change in the follicular phase. As a woman approaches menopause, the
frequency of ovulation decreases from 13 to 14 times per year to 11 to 12 times
per year. With advancing reproductive age, ovulation frequency may decrease to
3 to 4 times per year.
With the change in reproductive
cycle length and fre-quency, there are concomitant changes in the plasma
con-centration of FSH and LH. More FSH is required to stimulate follicular
maturation. Beginning in the late 30s and early 40s, the concentration of FSH
begins to increase from normal cyclic ranges (6–10 IU/L) to perimenopausal
levels (14–24 IU/L). During this period, women begin to experience symptoms and
signs of decreasing estrogen levels. Levels of FSH are 30 IU/L or more at
menopause.
Hot Flushes and Vasomotor Instability
Coincident with the change in reproductive cycle length and frequency, the hot flush is the first physical manifestation of decreasing ovarian function and is a symptom of vasomotor instability.
Hot flushes are recurrent,
transient episodes of flushing, perspiration, and a sensation ranging from
warmth to intense heat on the upper body and face, sometimes fol-lowed by
chills. When they occur during sleep and are asso-ciated with perspiration,
they are termed night sweats.
Occasional hot flushes begin several years before actual menopause. Other
conditions that can cause hot flushes include thyroid disease, epilepsy,
infection, and use of cer-tain drugs.
The hot
flush is the most common symptom of decreased estrogen production and is
considered one of the hallmark signs of perimenopause. However,
its incidence varies widely. SomeU.S. studies have found that about 75% of
women experi-enced hot flushes during the transition from the peri-menopause to
postmenopause. Outside the United States, rates vary even more widely, from
about 10% in Hong
Reasons
for these differences are unknown. In the United States, prevalence rates also
differ among racial and ethnic groups, with African-Americans most frequently
reporting symptoms (45.6%), followed by Hispanics (35.4%), whites (31.2%), Chinese
(20.5%), and Japanese (17.6%). More recent studies seem to indicate that
differences in body mass index (BMI) would be a more reliable indicator of the
incidence of hot flushes.
Hot flushes have a rapid onset
and resolution. When a hot flush occurs, a woman experiences a sudden sensation
of warmth. The skin of the face and the anterior chest wall become flushed for
approximately 90 seconds. With reso-lution of the hot flush, a woman feels cold
and breaks out into a “cold sweat.” The entire phenomenon lasts less than 3
minutes. The exact cause of hot flushes has not been determined, although it
seems that declining estradiol-17β
secretion by the ovarian follicles plays a significant role. As a woman
approaches menopause, the frequency and inten-sity of hot flushes increase. Hot
flushes may be disabling, especially at night. When perimenopausal and
post-menopausal women receive hormone therapy, hot flushes usually resolve in 3
to 6 weeks. If a menopausal woman does not receive hormone therapy, hot flushes
usually resolve spontaneously within 2 to 3 years, although some women
experience them for 10 years or longer.
Sleep Disturbances
Declining estradiol levels induce
a change in a woman’s sleep cycle so that restful sleep becomes difficult and
for some, impossible. The latent phase of sleep (i.e., the time required to
fall asleep) is lengthened; the actual period of sleep is shortened. Therefore,
perimenopausal and post-menopausal women complain of having difficulty falling
asleep and of waking up soon after going to sleep.
Sleep
disturbances are one of the most common and disabling effects of menopause.
Women with marked sleep
aberration are often tense and irritable and have difficulty with concentration
and inter-personal relationships. With hormone therapy, the sleep cycle is
restored to the premenopausal state.
Vaginal Dryness and Genital Tract Atrophy
The
vaginal epithelium, cervix, endocervix, endometrium, myo-metrium, and
uroepithelium are estrogen-dependent tissues. With decreasing estrogen production,
these tissues become atrophic, re-sulting in various symptoms. The
vaginal epithelium becomesthin and cervical secretions diminish. Women
experience vaginal dryness while attempting or having sexual inter-course,
leading to diminished sexual enjoyment and dys-pareunia. Atrophic vaginitis also may present with itching and burning. The
thinned epithelium is also more suscep-tible to becoming infected by local
flora. This discomfort can be relieved with systemic or topical hormone therapy
or the topical use of estrogen.
The endometrium also becomes
atrophic, sometimes resulting in postmenopausal spotting. The paravaginal
tis-sues that support the bladder and rectum become atrophic. When this is
combined with the effects of child bearing, it can result in loss of support
for the bladder (cystocele) and rectum (rectocele). In addition, uterine
prolapse is more common in the hypoestrogenic patient. Because of atrophy of
the lining of the urinary tract, there may be symptoms of dysuria and urinary
frequency, a condition called atrophic
urethritis. Hormone therapy can relieve the symptoms ofurgency, frequency,
and dysuria. Loss of support to the ure-throvesical junction may result in
stress urinary inconti-nence; in some cases, hormone therapy plus pelvic muscle
(Kegel) exercises may relieve some of these symptoms.
Mood Changes
Perimenopausal and postmenopausal
women often com-plain of volatility of affect. Some women experience
depres-sion, apathy, and “crying spells.” These feelings may be related to
menopause, to sleep disturbances, or both. The physician should provide
counseling and emotional support as well as medical therapy, if indicated. Although sex steroidhormone receptors are
present in the central nervous system, there is insufficient evidence about the
role of estrogens in central ner-vous system function.
Skin, Hair, and Nail Changes
Some
women notice changes in their hair and nails with the hor-monal changes of
menopause. Estrogen influences skin thick-ness. With declining
estrogen production, the skin tends to become thin, less elastic, and
eventually more susceptible to abrasion and trauma. Estrogen stimulates the
production of the sex hormone-binding globulin, which binds androgens and
estrogens. With declining estrogen production, less sex hormone-binding
globulin is available, thus increasing the level of free testosterone.
Increased testosterone levels may result in increased facial hair. Moreover,
changes in estro-gen production affect the rate of hair shedding. Hair from the
scalp is normally lost and replaced in an asynchronous way. With changes in
estrogen production, hair is shed and replaced in a synchronous way, resulting
in the appearance of increased scalp hair loss. This is a self-limiting
condition and requires no therapy, but patients do require reassur-ance. Nails
become thin and brittle with estrogen depriva-tion, but are restored to normal
with estrogen therapy.
Osteoporosis
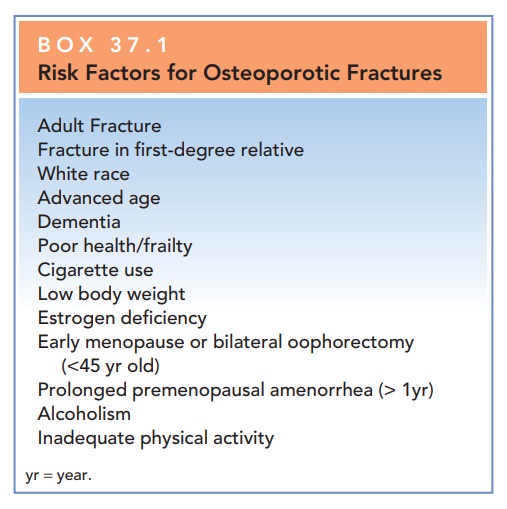
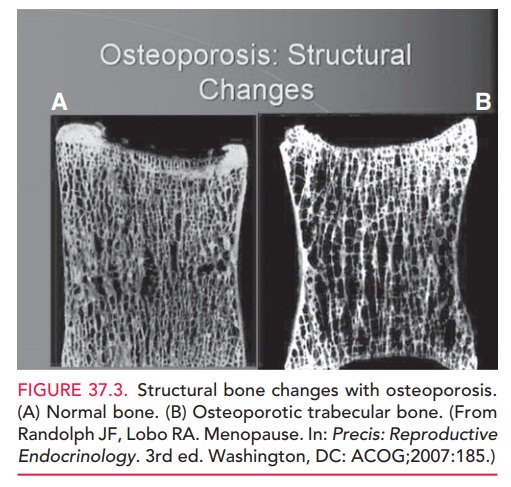
Bone
demineralization is a natural consequence of
aging.Diminishing bone density occurs in both men and women. However, the onset
of bone demineralization occurs 15 to 20 years earlier in women than in men by
virtue of accel-eration after ovarian function ceases. Bone demineraliza-tion
not only occurs with natural menopause, but also has been reported in association
with decreased estrogen pro-duction in certain groups of young women (such as
those with eating disorders or elite athletes). Other factors con-tribute to
the risk of osteoporosis (Box 37.1).
Estrogen receptors are present in
osteoblasts, which suggests a permissive and perhaps even an essential role for
estrogen in bone formation. Estrogen
affects the developmentof cortical and trabecular bone, although the effect on
the latter
Hormone therapy,
especially whencombined with appropriate calcium supplementation and
weight-bearing exercise, can help slow bone loss in meno-pausal women.
Weight-bearing activity such as walking for as little as 30 minutes a day
increases the mineral content of older women.
Calcium
supplementation is beneficial to prevent bone loss; 1500 mg of daily calcium
intake for menopausal women is rec-ommended. Calcium
therapy combined with estrogen
In
addition, for those with lim-ited sun exposure or those lacking other dietary
sources, supplementation with vitamin D should be considered: 10 μg from ages
of 51 to 70; 15 μg, older than 71.
Progressive, linear decrease in
bone mineral mass is noted in women who do not receive hormone therapy in the
first 5 to 10 years following menopause. When hor-mone therapy is initiated
before or at the time of meno-pause, bone density loss is greatly reduced.
Hormone therapy begun in a woman 5 or more years after menopause may still have
a positive effect on bone density loss. How-ever,
osteoporosis is not the primary indication for hormone therapy. Several
bisphosphonates such as alendronate,ibandronate, or risedronate can be used for
the manage-ment of menopause-associated bone loss. These agents reduce bone
resorption through the inhibition of osteoclas-tic activity (Table 37.3).
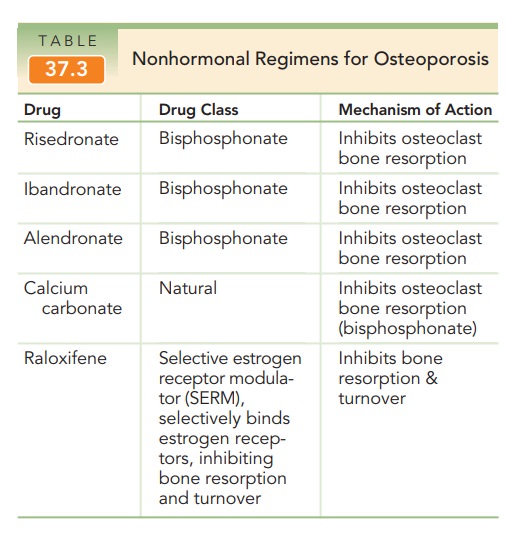
Selective
estrogen receptor modulators (SERMs) provide another nonhormonal management
option. Most estrogenicresponses are mediated in the body
by one of two receptors, either ER (alpha) or ER (beta). SERMs are ER ligands,
which act like estrogens in some tissues but block estrogen action in others.
Examples include tamoxifen and raloxifene, which exhibit ER antagonist activity
in the breast but ago-nist activity in the bone. As with the bisphosphonates,
they also lack the capabilities of mitigating many of the other estrogen
deprivation symptoms, such as hot flushes and sleeplessness, and may even
exacerbate these symptoms.
Cardiovascular Lipid Changes
With perimenopause, changes occur in the cardiovascular lipid profile.
Total cholesterol increases, high-density lipoprotein (HDL) cholesterol decreases, and
low-density lipoprotein (LDL) cholesterol increases. Hormone therapy may
pro-mote changes in the lipid profile that are favorable to the cardiovascular
system. Retrospective case control studies suggest that estrogens have a
cardioprotective effect. However, recent data from the Women’s Health
Initiative (WHI) suggest that no such protection exists in placebo control
clinical trials, though these trials have been criti-cized because of the late
onset of treatment following menopause. At
this time, hormone therapy should not beoffered to patients with the primary
goal of protection against heart disease.
Box 37.1
Risk Factors for Osteoporotic Fractures
Adult Fracture
Fracture in first-degree relative
White race
Advanced age
Dementia
Poor health/frailty
Cigarette use
Low body weight
Estrogen deficiency
Early menopause or bilateral oophorectomy (<45 yr old)
Prolonged premenopausal amenorrhea (> 1yr)
Alcoholism
Inadequate physical activity
yr = year.
Related Topics