Chapter: Obstetrics and Gynecology: Menopause
Menstruation and Menopause
Menopause
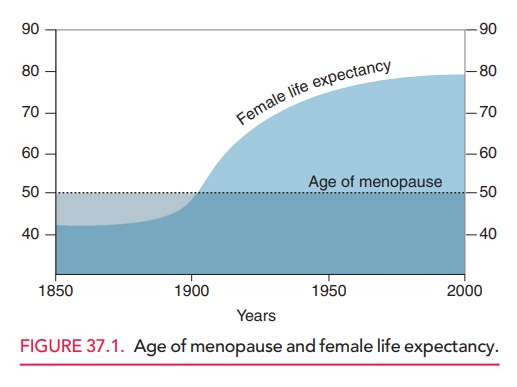
Menopause is the permanent cessation of menses afterM cessation of estrogen production.Perimenopauseis theperiod before menopause, i.e., the transition
from the reproductive to the nonreproductive years. The time period dur-ing
which the changes of menopause occur is called the climac-teric. An increasing
proportion of American women areincluded in these groups, because the female
life expectancy has lengthened and the number of women in this age group is
expanding (Fig. 37.1). Many women are expected to live 30 to 35 years—one third
of their life expectancy—after menopause.
MENSTRUATION AND MENOPAUSE
Whereas male gametes are renewed
on a daily basis, female gametes are of a fixed number that is progressively
reduced throughout a woman’s reproductive life. At the time of birth, the
female infant has approximately 1 to 2 million oocytes; by puberty, she has
approximately 400,000 oocytes remaining. By age 30 to 35, the number of oocytes
will have decreased to approximately 100,000. For the remain-ing reproductive
years, the process of oocyte maturation and ovulation becomes increasingly
inefficient.
A woman ovulates approximately
400 oocytes during her reproductive years. The process of oocyte selection is complex and new information is making the
process clearer. During the reproductive cycle, a cohort of oocytes is
stim-ulated to begin maturation, but only 1 or 2 dominant folli-cles complete
the process and are eventually ovulated.
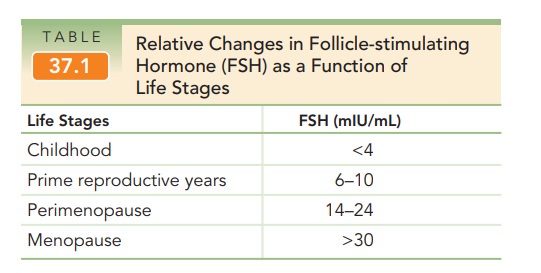
Follicular
maturation is induced and stimulated bythe pituitary release
of the follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FSH
binds to its receptors in the follicular membrane of the oocyte and stimulates
follicular maturation, providing estradiol (E2), which is the major
estrogen of the reproductive years. LH stimulates the theca luteal cells
surrounding the oocyte to produce androgens as well as estrogens and serves as
the triggering mechanism to induce ovulation. With advanc-ing reproductive age,
the remaining oocytes become increasingly resistant to FSH. Thus, plasma
concentra-tions of FSH begin to increase several years in advance of actual
menopause, when the FSH is generally found to be >30 mIU/mL (Table 37.1).
Menopause marks the end of a
woman’s natural repro-ductive life. The
average age for menopause in the United Statesis between 50 and 52 years of age
(median 51.5), with 95% ofwomen experiencing this event between the ages of
44 and
The age of menopause is not
influenced by the age of menarche, number of ovulations or pregnancies,
lactation, or the use of oral contraceptives. Race, socioeconomic sta-tus,
education, and height also have no effect on the age of menopause. Genetics and
lifestyle can affect the age of menopause. Undernourished women and smokers do
tend to have an earlier menopause, although the effect is slight. Approximately
1% of women undergo menopause before the age of 40, which is generally referred
to as prematureovarian failure.
Contrary to popular belief, the
ovaries of postmeno-pausal women are not quiescent. Under the stimulation of
LH, theca cell islands in the ovarian stroma produce hormones, primarily the
androgens testosterone and andro-stenedione. Testosterone appears to be the
major product of the postmenopausal ovary. Testosterone concentrations decline
after menopause, but remain two times higher in menopausal women with intact
ovaries than in those whose ovaries have been removed. Estrone is the predominant endogenous estrogen in postmenopausal
women. It is termed extragonadal
estrogen, because the concentration is directly related to body weight.
Androstenedione is con-verted to estrone in fatty tissue (Table 37.2).

Because
estrogen promotes endometrial proliferation, obese women have a higher risk of
endometrial hyperplasia and carcinoma. Conversely, slender women are at a
higher risk for menopausal symptoms.
Related Topics