Chapter: Obstetrics and Gynecology: Preconception and Antepartum Care
Subsequent Antenatal Visits - Preconception and Antepartum Care
SUBSEQUENT ANTENATAL VISITS
Regular monitoring of the mother
and fetus is essential for identifying complications that may arise during
preg-nancy and to provide assurance and support for mother and family,
especially for first pregnancies or when previ-ous pregnancies have been
complicated or had unfortunate outcomes. For a patient with a normal pregnancy,
periodic antepartum visits at 4-week intervals are usually scheduled until 28
weeks, at 2- to 3-week intervals between 28 and weeks, and weekly thereafter.
Patients with high-risk pregnancies or those with ongoing complications usually
are seen more frequently, depending on the clinical circum-stances. At each
visit, patients are asked about how they are feeling and if they are having any
problems, such as vaginal bleeding, nausea and vomiting, dysuria, or vagi-nal
discharge. After quickening, patients are asked if they continue to feel fetal
movement, and if it is the same or less since the last antepartum visit.
Decreased fetal movement after the time of fetal viability is a warning sign
requiring further evaluation of fetal well-being.
Every prenatal assessment
includes the following assessments:
·
Blood pressure
·
Weight
·
Urinalysis for albumin and
glucose
It is important to determine
baseline blood pressure and urine protein levels at the first antepartum visit.
Blood pressure generally declines at the end of the first trimester and rises
again in the third trimester. After 20 weeks of gestation, an increase in the
systolic pressure of more than 30 mm Hg or an increase in the diastolic
pressure of more than 15 mm Hg above the baseline level suggests (but alone
does not diagnose) gestational
hypertension. Comparison with baseline levels is necessary in order to
accurately dis-tinguish preexisting hypertension from hypertension asso-ciated
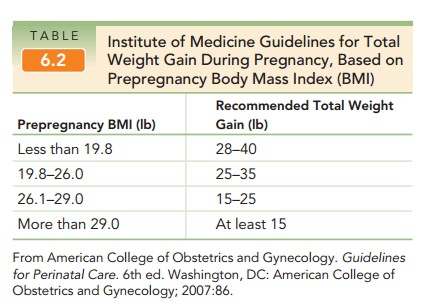
with pregnancy.Maternal weight is another important parameter to fol-low
through pregnancy, as weight gain recommendations differ for women of differing
prepregnancy body massindex (BMI). A
total weight gain of 25 to 35 lb is onlyappropriate for a woman of normal BMI
(see Table 6.2). The obese pregnant woman with a pregravid BMI >=30 is at risk for multiple
complications during pregnancy, including preeclampsia, gestational diabetes,
and need for cesarean delivery. Between monthly visits, a 3- to 4-lb weight
gain is generally appropriate for a woman of normal BMI. Significant deviation
from this trend may require nutritional assessment and further evaluation.
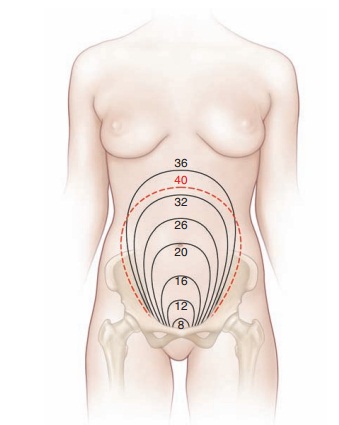
Obstetric physical findings made
at each visit include fundal height measurement, documentation of the pres-ence
and rate of fetal heart tones, and determination of the presentation of the
fetus. Until 18 to 20 weeks, the uterine size is generally stated as weeks’
size, such as “12 weeks’ size.” After 20 weeks of gestation (when the fundus is
pal-pable at or near the umbilicus in a woman of normal body habitus and a
singleton pregnancy in the vertex presenta-tion), the uterine size can be
assessed with the use of a tape measure, which is the fundal height measurement. In this procedure, the top of the
uterine fundus is identified and the zero end of the tape measure is placed at
this uppermost part of the uterus. The tape is then carried ante-riorly across
the abdomen to the level of the symphysis pubis. From 16 to 18 weeks of
gestation until 36 weeks of gestation, the fundal height in centimeters
(measured from the symphysis to the top of the uterine fundus) is roughly equal
to the number of weeks of gestational age in normal singleton pregnancies in
the cephalic presentation within an anatomically normal uterus (Fig. 6.1).
Until 36 weeks in the normal singleton pregnancy, the number of weeks of
gestation approximates the fundal height in centimeters. Thereafter, the fetus
moves downward into the pelvis beneath the symphysis pubis (“lightening,” or
engagement of the head into the true pelvis), so that the fundal height
measurement is increasingly unreliable.
Fetal
heart rate should be verified at every visit, bydirect
auscultation or by the use of a fetal Doppler ultra-
The normal fetal
heart rate is 110 to 160 bpm, with higher rates found in early pregnancy. The
maternal pulse may also be detected with the Doppler device, so simultaneous
palpation of maternal pulse and auscultation of fetal pulse may be necessary to
differentiate the two. Deviation from the normal rate or occasional arrhythmias
must be evaluated carefully.
Several determinations concerning
the fetus can be made by palpation of
the pregnant uterus, such as iden-tifying the presentation, or “presenting
part” of the fetus; that is, what part of the fetus is entering the pelvis
first. Before 34 weeks of gestation, breech, oblique, or trans-verse
presentations are not uncommon. The presentation of the fetus may also vary
from day to day. At term, more than 95% of fetuses are in the cephalic
presentation (head down). Approximately 3.5% are breech (bottom first), and 1%
are shoulder first. Unless the fetus is in a transverse lie (the long axis of
the fetus is not parallel with the mother’s long axis), the presenting part
will be either the head (ver-tex, cephalic) or the breech (buttocks).
The presentation of the fetus can
be appreciated on clinical exam with the use of Leopold maneuvers (see Figure 9.7, p. 112). In the first maneuver,
breech pre-sentation can be appreciated by outlining the fundus and determining
what part is present. The head is hard and well-defined by ballottement,
especially when the head is freely mobile in the fluid-filled uterus; the
breech is softer, less round, and, therefore, more difficult to outline. In the
second and third maneuvers, the examiner’s palms are placed on either side of
the maternal abdomen to deter-mine the location of the fetal back and small
parts. In the fourth maneuver, the presenting part is identified by exert-ing
pressure over the pubic symphysis. If a breech presen-tation persists at 36 and
38 weeks, the option of externalcephalic
version (ECV) should be discussed with thepatient. This procedure involves
turning the fetus from the breech presentation to a vertex presentation to
allow vaginal rather than cesarean delivery. It is contraindicated in the
presence of multifetal gestation, fetal compromise, uterine anomalies, and
problems of placentation.
Related Topics