Chapter: Obstetrics and Gynecology: Preconception and Antepartum Care
Specific Techniques of Fetal Assessment
SPECIFIC TECHNIQUES OF FETAL ASSESSMENT
Continued
evaluation of the fetus includes techniques for assess-ment of fetal (1)
growth, (2) well-being, and (3) maturity. These
tests must be interpreted in light of the clinical con-text and provide a basis
for management decisions.
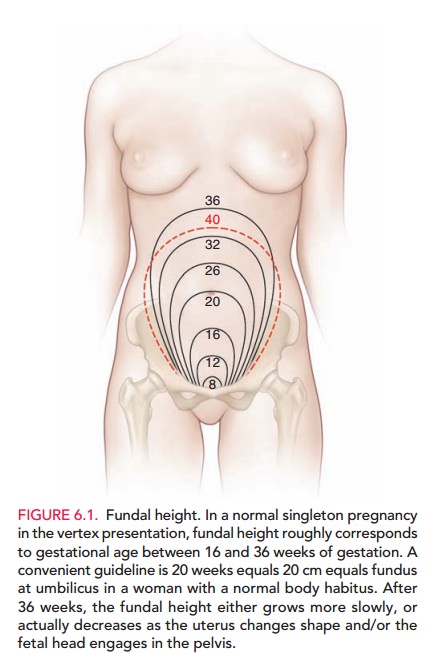
Assessment of Fetal Growth
Fetal growth can be assessed by
fundal height measurement, as the initial measure, and ultrasonography. The
increase in fundal height through pregnancy is predictable. If the fundal
height measurement is significantly greater than expected (i.e., large for gestational age [LGA]),
possible considerations include incorrect assessment of gestational age,
multiple pregnancy, macrosomia (large fetus), hyda-tidiform mole, or excess
accumulation of amniotic fluid (polyhydramnios). A fundal height measurement
less than expected, or small for
gestational age (SGA), suggests the possibility of incorrect assessment of
gestational age, hydatidiform mole, fetal growth restriction, inadequate
amniotic fluid accumulation (oligohydramnios), or even intrauterine fetal
demise. Deviation in fundal height mea-surement should be closely evaluated.
Ultrasound is the most valuable
tool in assessing fetal growth. Ultrasound
has many potential uses for both fetal datingand identifying any fetal
anomalies. In early pregnancy, deter-mination of the gestational-sac
diameter and the crown-to-rump length correlates closely with gestational age.
Later in pregnancy, measurement of the biparietal diameter of the skull, the
abdominal circumference, the femur length, and the cerebellar diameter can be
used to assess gestational age and, using various formulas, to estimate fetal
weight.
Assessment of Fetal Well-Being
Assessment of fetal well-being includes subjective
mater-nal perception of fetal activity and several objective tests using
electronic fetal monitoring and ultrasonography. Tests of fetal well-being have
a wide range of use, includ-ing the assessment of fetal status at a particular
time and prediction of future well-being for varying time intervals, depending
on the test and the clinical situation.
Evaluation
of fetal activity is a common
indirect measure of fetal well-being. A variety
of methods can be used to quan-tify fetal activity, including the time
necessary to achieve a certain number of movements each day, or counting the
number of movements (“kick counts”)
in a given hour. This type of testing is easily performed and involves the
patient in her own care. If the mother notices less move-ment, further
evaluation may be needed.
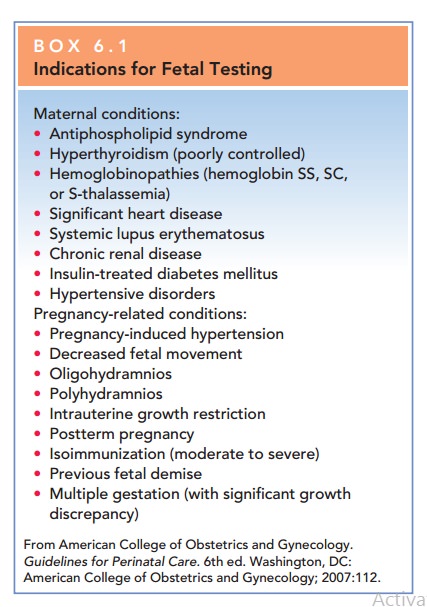
Fetal monitoring tests can
provide more objective information about fetal well-being. These tests include
the nonstress test (NST), contraction stress test (CST) (called the oxytocin
challenge test [OCT] if oxytocin is used), biophysical profile (BPP), and
ultrasonography of umbilical artery blood flow velocity. Although there is no
optimal time to initiate fetal testing, there are several maternal and
pregnancy-related indications (Box 6.1).
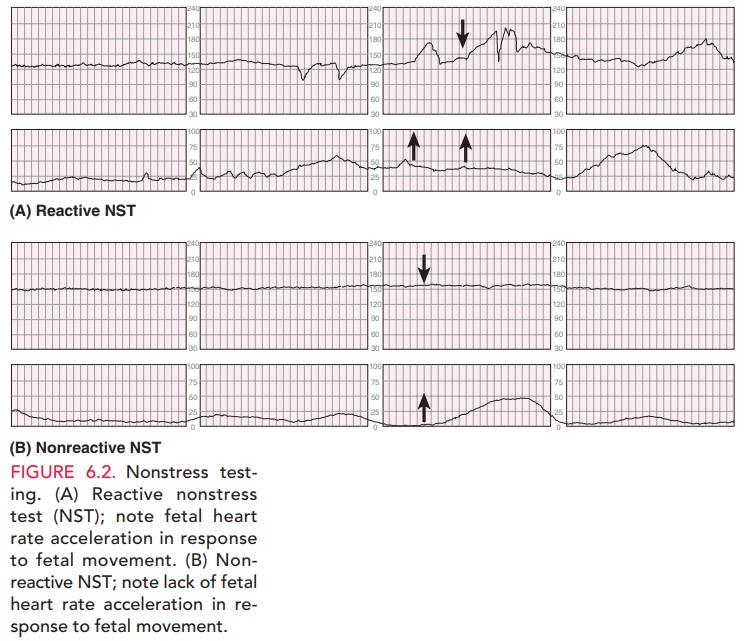
NONSTRESS TEST
The nonstress test measures the fetal heart rate, which is mon-itored with an external transducer for at least 20 minutes. Thepatient is asked to note fetal movement, usually accom-plished by pressing a button on the fetal monitor, which causes a notation on the monitor strip. The tracing is observed for fetal heart rate accelerations (Fig. 6.2). The results are considered reactive (or reassuring) if two or more fetal heart rate accelerations occur in a 20-minute period, with or without fetal movement discernible by the mother. A nonreactive (nonreassuring) tracing is one without suffi-cient heart rate accelerations in a 40-minute period. A non-reactive NST should be followed with further fetal assessment.
CONTRACTION STRESS TEST
Whereas
the NST evaluates the fetal heart rate response to fetal activity, the contraction stress test measures the
response of the fetal heart rate to the stress of a uterine contraction. During
auterine contraction, uteroplacental blood flow is temporar
A healthy fetus is able to compensate for this intermittent
decreased blood flow, whereas a fetus that is compromised may be unable to do
so. To perform a CST, a tocodynamometer is placed on the maternal abdomen along
with a fetal heart rate trans-ducer for a baseline tracing for 10 to 20
minutes. If there are no contractions, they are induced by nipple
self-stimulation or oxytocin (this test is called an OCT). A neg-ative (normal)
result is indicated if there is no change from the baseline fetal heart rate
and no fetal heart rate deceler-ations. If
decelerations occur, the results can be considered posi-tive, equivocal, or
unsatisfactory, depending on the pattern, frequency, and strength of the
deceleration.
These tests of fetal well-being
have a significant inci-dence of false-positive results (i.e., results
suggesting that the fetus is in jeopardy, though the fetus is actually
healthy). Forthis reason, the results of
these tests must be interpreted collectively, and the tests themselves repeated
to verify the results. When mul-tiple test results are reassuring, they
tend to rule out a prob-lem. When all results are nonreassuring, they tend to
signify the presence of a problem.
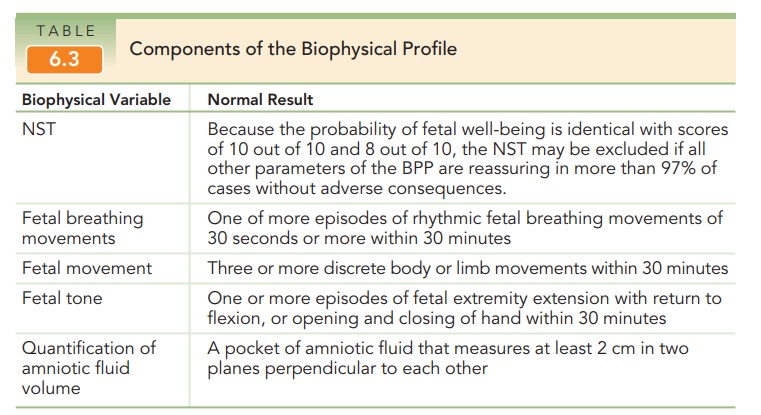
BIOPHYSICAL PROFILE
If an OCT is positive, evidence
to support fetal well-being, such as that provided by a biophysical profile (BPP), is sought. The BPP is a series of five
assessments of fetal well-being, each of which is given a score of 0 (absent)
or 2 (pres-ent) [Table 6.3]. The parameters include a reactive NST, the
presence of fetal breathing movements, the presence of fetal movement of the
body or limbs, the finding of fetal tone (flexed extremities as opposed to a
flaccid posture), and an adequate amount of amniotic fluid volume. A total
score of 8 to 10 is considered reassuring. A total score of 6 is equivocal and
generally should lead to delivery if the patient is at term. If the patient is
preterm, retesting within 12 to 24 hours may be appropriate. A score of 4 or
less is nonreassuring and warrants further evaluation and consideration of
delivery. Irrespective of the score, more fre-quent BPP testing or
consideration of delivery may be war-ranted when oligohydramnios is present.1(p116)
Management based on the BPP depends not only on the score itself, but also on
the gestational age of the fetus.
Modified
BPP combines use of an NST and assessment of an amniotic fluid index (AFI). The
AFI is a semiquantita-tive, four-quadrant assessment of amniotic fluid depth. Theimportance
of adequate amniotic fluid volume is
well-established. Diminished amniotic fluid is thought to represent decreased
fetal urinary output caused by chronic stress and shunting of blood flow away
from the kidneys. The decreased amniotic fluid provides less sup-port for the
umbilical cord, which may be more com-pressed, reducing blood flow. The modified BPP is lesscumbersome than the
BPP and appears to be as predictive of fetal well-being.
DOPPLER ULTRASOUND OF UMBILICAL ARTERY
Umbilical
Artery Doppler flow ultrasonography is
anoninvasive technique to assess resistance to blood flow in the placenta. It
can be used in conjunction with other biophysical tests in high-risk
pregnancies associated with suspected intrauterine growth restriction.
Umbilical cord Doppler flow velocimetry is based on the characteristics of the
systolic blood flow and the diastolic blood flow. The most commonly used index
to quantify the flow velocity waveform is the systolic/diastolic ratio. As
peripheral resis-tance increases, diastolic flow decreases and may become
absent or reserve, and the systolic/diastolic ratio increases. Reversed
end-systolic flow can be seen with severe cases of intrauterine growth
restriction secondary to uteroplacen-tal insufficiency and may suggest
impending fetal demise.
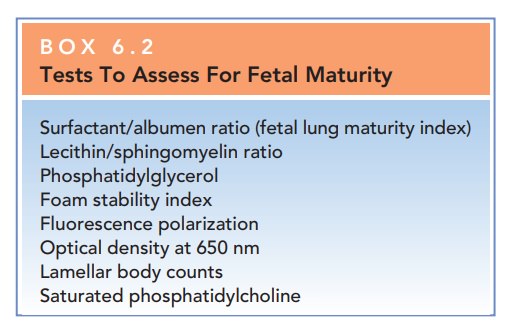
Assessment of Fetal Maturity
Fetal maturity should always be
taken into consideration when delivering a fetus electively or preterm in
high-risk pregnancies. Several tests are available to assess fetal matu-rity
(Box 6.2). Because the respiratory system is the last fetal system to mature
functionally, many of the tests avail-able to assess fetal maturity focus on
this organ system. Several phospholipids, collectively known as surfactant, enter the amniotic fluid
where they can be obtained by amniocentesis and measured. Surfactant is
necessary for normal lung function, as it maintains the patency of the alveolar
sacs. The ratio of two phospholipids, lecithin
andsphingomyelin, called the L/S
ratio, has been used todetermine fetal lung maturity, but other tests are
rapidly replacing use of this ratio. Another important phospholipid contained
in the surfactant complex is phosphatidylglyc-erol
(PG), a marker of complete pulmonary maturationthat is present after 35
weeks of gestation.
Neonates delivered before their
lungs have matured are at risk of respiratory
distress syndrome (RDS), a serious and life-threatening condition caused by
lack of surfactant. RDS in newborns is manifest by signs of res-piratory
failure—grunting, chest retractions, nasal flar-ing, and hypoxia—possibly
leading to acidosis and death. Management consists of skillful support of
ventilation and correction of associated metabolic disturbances until the
neonate can ventilate without assistance. Adminis-tration of synthetic or
semi-synthetic surfactant to the neonate has resulted in improved outcomes for
infants with RDS.
Results of pulmonary function
tests that indicate immaturity do not have a high predictive value for RDS.
Because no test indicating maturity can completely elimi-nate the risk of RDS
or other neonatal complications, the risk of adverse fetal outcome following
delivery must be weighed against the potential risk of allowing the pregnancy
to continue
Related Topics