Chapter: Obstetrics and Gynecology: Preconception and Antepartum Care
Antepartum Patient Education
ANTEPARTUM PATIENT EDUCATION
Plans for the antepartum,
intrapartum, and postpartum periods provide an opportunity for patient
education and interaction. The Antepartum Record in Appendix C provides a list
of the issues to be discussed during ante-partum care.
Employment
A woman with an uncomplicated
pregnancy can usually continue to work until the onset of labor. In a normal
pregnancy, there are few restrictions concerning work, although it is
beneficial to allow moderate activity and to allow for periods of rest. Strenuous
work (standing or repetitive, strenuous, physical lifting) is best avoided.
A period of 4 to 6 weeks
generally is required for a woman’s physical condition to return to normal.
However, the patient’s individual circumstances may be a factor in determining
when she returns to work. The length of a woman’s leave from work can depend on
whether there are pregnancy or delivery complications, the work involved, the
employer attitude, the rules of the health care system under which the patient
receives care, and the wishes of the patient. The Federal Family and Medical
Leave Act and state laws should be consulted to determine the family and
medical leave that is available.1(p118)
Exercise
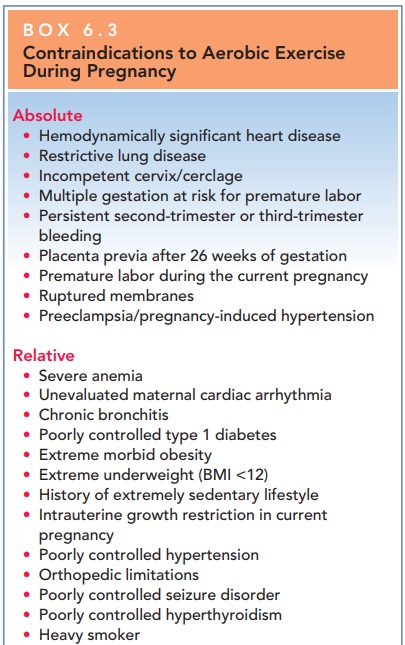
In the absence of either medical
or obstetric complications, up to 30 minutes of moderate exercise per day on
most if not all days of the week is acceptable (Box 6.3). Each sport should be
reviewed for its potential risk, and activities with a high risk for falling or
for abdominal trauma should be avoided.
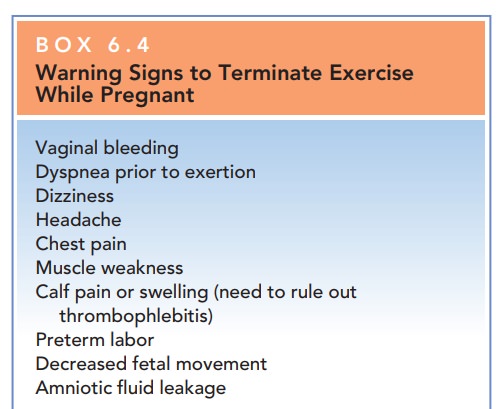
Overly strenuous exercise,
especially for prolonged periods, should be avoided. Patients unaccustomed to
reg-ular exercise should not undertake vigorous new programs during pregnancy. Supine exercises should be
discon-tinued after the first trimester to minimize circulatory changes brought
on by pressure of the uterus on the vena cava. Any activity should be
discontinued if discomfort, significant shortness of breath, or pain in the
chest or abdomen appears (Box 6.4). Changes in body contour and balance will
alter the advised types of activities; abdominal trauma should be avoided.
Sitting in a hot tub or sauna after exercise is of con-cern to pregnant women. Possible hyperthermia may be teratogenic. Pregnant women might reasonably be advised to remain in saunas for no more than 15 minutes, and in hot tubs for no more than 10 minutes. In a hot tub, if a woman’s head, arms, shoulders, and upper chest are not submerged, there is less surface area to absorb heat.
Nutrition and Weight Gain
Concerns about adequate nutrition
and weight gain dur-ing pregnancy are common. Poor nutrition, obesity, and food
faddism are associated with poor perinatal outcome. Pica, or an inclination for nonnutritional substances suchas ice,
food starch, or clay or dirt, is often associated with anemia.
A complete nutritional assessment
is an important part of the initial antepartum assessment, including history of
dietary habits, special dietary issues or concerns, and weight trends. Anorexia
and bulimia increase risks for associated
Calculation of BMI is useful because it relates weight to height, allowing for
a better indirect measurement of body fat distribution than is obtained with
weight alone. Further, because of the “personalized nature” of an individual’s
BMI, it is often more useful in teaching a patient about diet and weight issues
than an abstract table.
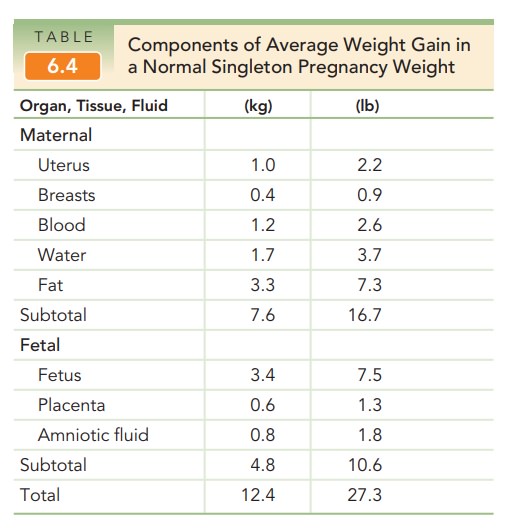
Recommendations for total weight
gain during preg-nancy and the rate of weight gain per month appropriate to
achieve it may be made based on a body mass index calculated for the
prepregnancy weight (see Table 6.3). The components that make up the average
weight gain in a normal singleton pregnancy are listed in Table 6.4. The
maternal component of this weight gain starts in the first trimester and
increases linearly after the second trimester. Fetal growth is most rapid in the
second half of pregnancy, with the normal fetus tripling its weight in the last
12 weeks.
Published recommended daily allowances (RDAs) for protein, minerals, and
vitamins are useful approxima-tions. It should be kept in mind, however, that
the RDAs are a combination of estimates and are values adjusted near the top of
the normal ranges to encompass the estimated needs of most women. Thus, many
women have an adequate diet for their individual needs, even though it does not
supply all the RDAs. Vitamin supplementation is appropriate for spe-cific
therapeutic indications, such as a patient’s inability or unwillingness to eat
a balanced, adequate diet, or clinical demonstration of a specific nutritional
risk. Except for iron, mineral supplementation is likewise not required in
other-wise healthy women; the National Academy of science rec-ommends 27 mg of
iron supplementation.
Financial problems, the inability
to get to a grocery store, and foodstuffs unique to a patient’s social group
that differ in substantial quantitative ways with respect to important
nutrients, may prevent some women from obtaining adequate nutrition, even if
the volume of food-stuffs seems sufficient. The WIC Federal Supplemental food
program, food stamp programs, and Aid for Families with Dependent Children are
resources that may help in these situations.
Breastfeeding
The benefits of breastfeeding include, for the newborn,
excellent nutrition and provision of immunologic protec-tion; and, for the
mother, more rapid uterine involution, economy, maternal–child bonding, to some
extent natural contraception, and, often, more rapid weight loss associ-ated
with extra calorie expenditure. Contraindications to breastfeeding include
certain maternal infections and use of medications. It is important to support
a woman who chooses not to breastfeed. The use of breast pumps and milk storage
may allow a mother to continue breastfeed-ing while continuing to work.
Sexual Activity
Sexual intercourse is not
restricted during a normal preg-nancy, although advice about more comfortable
positions in later pregnancy may be appreciated—for example, side-to-side or
the female-superior position. Sexual activity may be restricted or prohibited
under certain high-risk circumstances, such as known placenta previa, premature
rupture of membranes, or actual or history of preterm
labor (or delivery). Education of
the patient (and partner) about safe sex practices is as important in
antepartum as in regular gynecologic care.
Travel
Up to 36 weeks of gestation,
women can safely fly. Air travel is not recommended for women who have medical
or obstetric complications, such as hypertension, poorly controlled diabetes
mellitus, or sickle cell disease. This recommendation is not due to substantial
risk to either mother or fetus, but because of the likelihood that labor may
ensue away from home and customary health care providers. If a long trip near
term is planned, it is useful for the patient to carry a copy of her obstetric
record in case she requires obstetric care. When traveling, patients are
advised to avoid long periods of inactivity, such as sit-ting. Walking every 1
to 2 hours, even for short periods, promotes circulation, especially in the lower
legs, and decreases the risk of venous stasis and possible thrombo-embolism.
Additionally, preventive antiemetic medicine should be considered for pregnant
women with increased nausea. Education about the regular use of a seat belt is
especially important, with the seat belt worn low on the hip bones, between the
protuberant abdomen and the pelvis.
Teratogens
Many patient inquiries concern
the teratogenic potential of environmental exposures. Major birth defects are apparent at birth in
2% to 3% of the general population, and the possible occurrence of fetal
malformations or mental retardation is a frequent cause of anxiety among
pregnant women. Of these, about 5% may be a result of maternal exposure to
drugs or environmental chemicals, and only approximately 1% can be attributed
to pharma-ceutical agents. The most important determinants of the developmental
toxicity of an agent are timing, dose, and fetal susceptibility. Many agents
have teratogenic effects only if taken while the susceptible fetal organ system
is forming.
The health care provider may wish
to consult with or refer such patients to health care professionals with
special knowledge or experience in teratology and birth defects. The
Organization of Teratology Information Services provides information on
teratology issues and exposures in pregnancy (www.otis pregnancy.org).
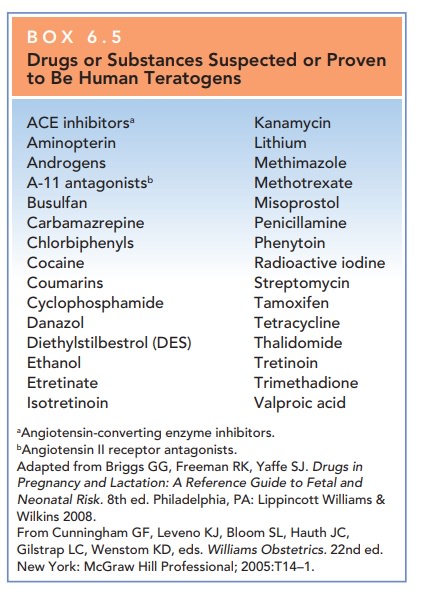
MEDICATIONS
Very few medications have been
proven to be true human teratogens (Box 6.5). Most commonly prescribed
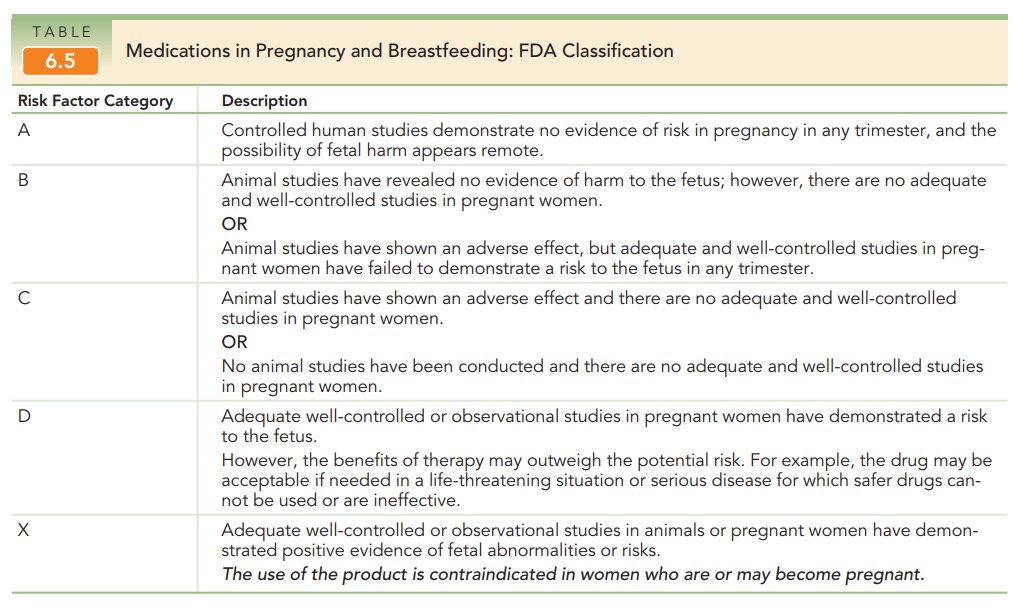
medica-tions are relatively safe in pregnancy. The Food and Drug Administration
assigns medications a pregnancy risk factor
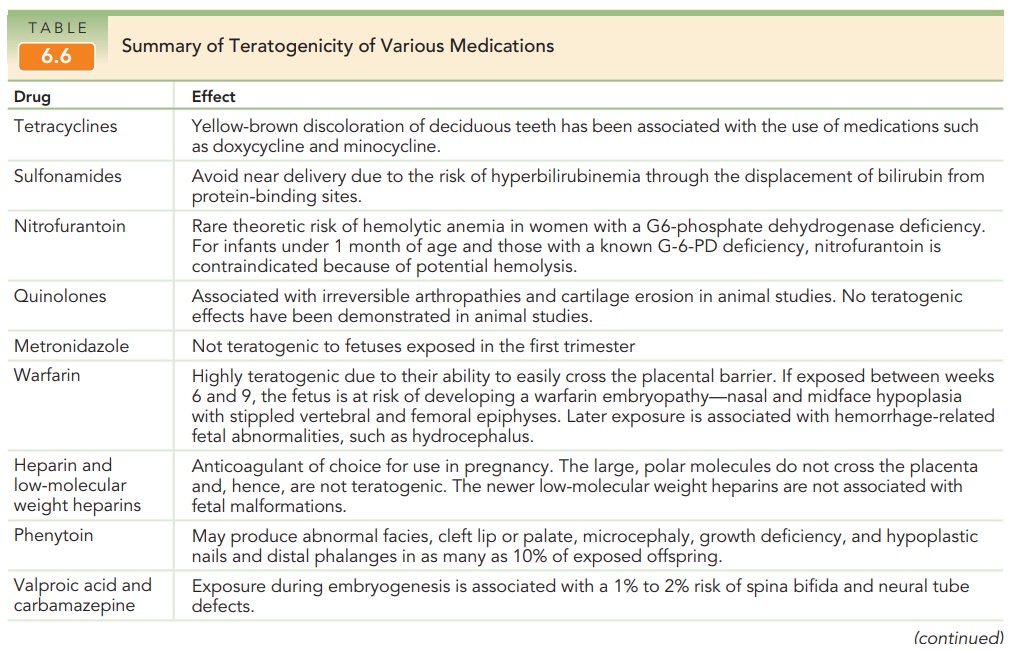
These pregnancy risk factors help guide
the appropriate use of medications in pregnancy (see Table 6.5). Table 6.6
provides a summary of the teratogenicity of many common medications.
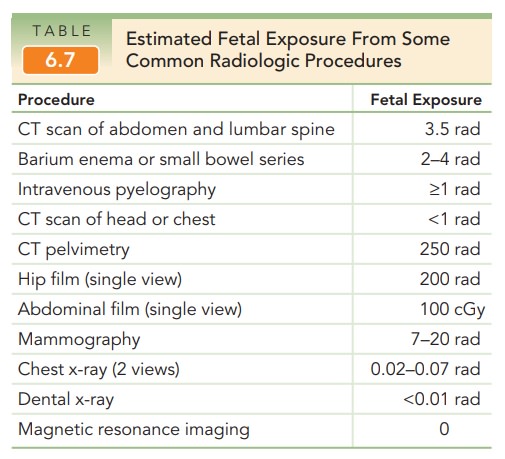
IONIZING RADIATION
Ionizing radiation exposure is
universal; most radiation originates from beyond the earth’s atmosphere, from
the land, and from endogenous radionuclides. The total radiation exposure from
these sources is approximately 125 mrads per year. Although radiation exposure
has the potential to cause gene mutations, growth impairment, chromosome damage
and malignancy, or fetal death, large doses are required to produce discernible
fetal effects. Large doses (10 rads) during the first two weeks after
fertilization are required to produce a deleterious effect. In the first trimester,
25 rads are required to pro-duce detectable damage, and 100 rads are required
later in pregnancy. Diagnostic radiation usually exposes the fetus to much less
than 5 rads, depending on the number of radiographs taken and the maternal site
examined (Table 6.7).
METHYL MERCURY
Industrial pollution is the major
source of mercury entry in our ecosystem. Large fish, such as tuna, shark, and
king mackerel, retain higher levels of mercury from the smaller fish and
organisms they consume. Hence, women who eat these fish are storing high levels
of mercury.
The FDA recommends that pregnant
women limit their ingestion of albacore tuna to 6 ounces per week or to 12
ounces per week of fish and shellfish varieties thought to be low in mercury.
HERBAL REMEDIES
Herbal remedies are not regulated
as prescription or over-the-counter drugs, the identity and quantity of their
ingredients are unknown, and there are virtually no studies of their
teratogenic potential. Because it is not possible to assess their safety, pregnant
women should be counseled to avoid these substances. Remedies contain-ing
substances with pharmaceutical properties that could theoretically have adverse
fetal affects include the following:
· Echinacea—causes
fragmentation of hamster sperm at high concentrations
· Black
cohosh—contains a chemical that acts like an estrogen
· Garlic
and willow barks—have anticoagulant properties
· Ginkgo—can
interfere with effects of monamine oxidase inhibitors; has anticoagulant
effects
· Real
licorice—has hypertensive and potassium-wasting effects
· Valerian—intensifies
the effects of prescription sleep aids
· Ginseng—interferes
with the effects of monamine oxidase inhibitors
· Blue
cohosh and pennyroyal—stimulate uterine muscu-lature; pennyroyal also can cause
liver damage, renal fail-ure, disseminated intravascular coagulation, and
maternal death
ALCOHOL
Alcohol is the most common
teratogen to which a fetus is exposed, and alcohol consumption during pregnancy
is a leading preventable cause of mental retardation, develop-mental delay, and
birth defects in the fetus. There is substan-tial evidence that fetal toxicity
is dose-related and that the exposure time of greatest risk is the first
trimester. There is no established safe level of alcohol use during pregnancy.
Women who are pregnant or who are at risk for pregnancy should not drink
alcohol. Although consumption of small amounts of alcohol early in pregnancy is
unlikely to cause serious fetal problems, patients are best advised to refrain
from alcohol entirely.
Fetal
alcohol syndrome (FAS) is a congenital syn-drome
characterized by alcohol use during pregnancy and by three findings:
·
Growth restriction (which may
occur in the prenatal period, the postnatal period, or both)
·
Facial abnormalities, including
shortened palpebral fissures, low-set ears, midfacial hypoplasia, a smooth
philtrum, and a thin upper lip
·
Central nervous system
dysfunction, including micro-cephaly; mental retardation; and behavioral
disorders, such as attention deficit disorder
The exact risk incurred by
maternal alcohol use is difficult to establish, because the complex pattern of
symptoms asso-ciated with FAS can make diagnosis difficult. Consumption of 8 or
more drinks daily throughout pregnancy confers a 30% to 50% risk of having a
child with FAS. However, even low levels of alcohol consumption (two or fewer
drinks per week) have been associated with increased aggressive behavior in
children.
Tobacco Use
The risks of smoking during pregnancy have been well-established and include
risks to the fetus such as intrauterine growth restriction, low birth weight,
and fetal mortality. It is important for the obstetrician to take advantage of
the pre-natal visits to educate patients about the risks of smoking for both
themselves and their newborns and to coordinate appropriate resources to help
patients quit. Counseling pro-grams are available to help patients quit
smoking. Nicotine replacement products may be considered, although their safety
in pregnancy has not been documented.
Substance Abuse
The use of illicit substances by
women of childbearing age has led to an increased number of neonates having had
in utero exposure and subsequent risk of adverse effects from a variety of
drugs. Fetal drug exposure often is unrecog-nized because of the lack of overt
symptoms or structural anomaly following birth.
Illicit drugs may reach the fetus
via placental transfer or may reach the newborn through breast milk. The
spe-cific effect on the fetus and newborn varies with the respec-tive
substances. An opiate-exposed fetus may experience withdrawal symptoms in utero
if the woman stops or when the woman goes through withdrawal, either
voluntarily or under supervision, or after birth when the delivery by way of
the placenta ceases.
Universal screening, using biologic
specimens, of women and newborns for substance abuse is not recom-mended.
However, all pregnant women should be asked at their first prenatal visit about
past and present use of alcohol, nicotine, and other drugs, including
recreational use of prescription and over-the-counter medications. Use of
specific screening questionnaires may improve detection rates. A woman who
acknowledges use of these substances should be counseled about the perinatal
implications of their use during pregnancy, and offered referral to an
appropriate drug-treatment program if chemical dependence is sus-pected.
Careful follow-up during the postpartum period is also recommended.
Related Topics