Chapter: Essentials of Psychiatry: Anxiety Disorders: Social and Specific Phobias
Social and Specific Phobias: Diagnosis and Differential Diagnosis
Diagnosis and Differential Diagnosis
Panic disorder with agoraphobia may easily be misdiagnosed as social
phobia or a specific phobia (especially the situational type). For example,
many patients with panic disorder avoid a variety of social situations because
of anxiety about having oth-ers notice their symptoms. In addition, some
individuals with panic disorder may avoid circumscribed situations, such as
fly-ing, despite reporting no other significant avoidance. Four vari-ables
should be considered in making the differential diagnosis: 1) type and number
of panic attacks; 2) focus of apprehension; 3) number of situations avoided;
and 4) level of intercurrent anxiety.
Patients with panic disorder experience unexpected panic attacks and
heightened anxiety outside of the phobic situation, whereas those with specific
and social phobias typically do not. In addition, individuals with panic
disorder are more likely than those with specific and social phobias to report
fear and avoid-ance of a broad range of situations typically associated with
agoraphobia (e.g., flying, enclosed places, crowds, being alone, shopping
malls). Finally, patients with panic disorder are typi-cally concerned only
about the possibility of panicking in the phobic situation or about the
consequences of panicking (e.g., be-ing embarrassed by one’s panic symptoms).
In contrast, individu-als with specific and social phobias are usually
concerned about other aspects of the situation as well (e.g., being hit by
another driver, saying something foolish).
Consider two examples in which the differential diagnosis with panic
disorder might be especially difficult. First, individu-als with claustrophobia
are typically extremely concerned about being unable to escape from the phobic
situation as well as being unable to breathe in the situation. Therefore, like
patients with panic disorder and agoraphobia, they usually report heightened
anxiety about the possibility of panicking. The main variable to consider in
such a case is the presence of panic attacks outside of claustrophobic
situations. If panic attacks occur exclusively in enclosed places, a diagnosis
of specific phobia might best de-scribe the problem. In contrast, if the
patient has unexpected or uncued panic attacks as well, a diagnosis of panic
disorder might be more appropriate.
A second example is a patient who avoids a broad range of situations
including shopping malls, supermarkets, walking on busy streets, and various
social situations including parties, meetings and public speaking. Without more
information, this patient’s problem might appear to meet criteria for social
pho-bia, panic disorder with agoraphobia, or both diagnoses. As men-tioned
earlier, patients with panic disorder often avoid social situ-ations because of
anxiety about panicking in public. In addition, patients with social phobia
might avoid situations that are typi-cally avoided by individuals with
agoraphobia for fear of seeing someone that they know or of being observed by
strangers. To make the diagnosis in this case, it is necessary to assess the
rea-sons for avoidance.
Other diagnoses that should be considered before a diag-nosis of
specific phobia is assigned include post traumatic stress disorder (PTSD) (if
the fear follows a life-threatening trauma and is accompanied by other PTSD
symptoms such as reexperiencing the trauma), obsessive–compulsive disorder (if
the fear is related to an obsession, e.g., contamination), hypochondriasis (if
the fear is related to a belief that he or she has some serious illness),
separation-anxiety disorder (if the fear is of situations that might lead to
separation from the family, for example, traveling on an airplane without one’s
parents), eating disorders (if the fear is of eating certain foods but not
related to a fear of choking) and psy-chotic disorders (if the fear is related
to a delusion).
Social phobia should not be diagnosed if the fear is related entirely to
another disorder. For example, if an individual with obsessive–compulsive
disorder avoids social situations only be-cause of the embarrassment of having
others notice her or his excessive hand washing, a diagnosis of social phobia
would not be given. Furthermore, individuals with depression, schizoid
personality disorder, or a pervasive developmental disorder may avoid social
situations because of a lack of interest in spending time with others. To be
considered social phobia, an individual must avoid these situations
specifically because of anxiety about being evaluated negatively.
In the case of generalized social phobia, the diagnosis of avoidant
personality disorder should be considered as well. Indi-viduals with avoidant
personality disorder tend to display more interpersonal sensitivity and have
poorer social skills than social phobic patients without avoidant personality
disorder. Further-more, most studies suggest that the differences between
avoid-ant personality disorder and social phobia are more quantitative than
qualitative and that the former may simply be a more severe form of the latter.
Therefore, most patients who meet criteria for avoidant personality disorder
will meet criteria for social phobia as well.
Finally, social and specific phobias should be distinguished from normal
states of fear and anxiety. Many individuals report mild fears of circumscribed
situations or mild shyness in certain social situations. Others may report
intense fears of public speak-ing or heights but insist that these situations
rarely arise and that they have no interest in being in these situations. For
the crite-ria for a specific or social phobia to be met, the individual must
report significant distress about having the fear or must report significant
impairment in functioning.
A variety of factors should be considered in deciding whether a
patient’s fear exceeds the threshold necessary for a diagnosis of specific or
social phobia. To make the differential diagnosis between normal fears and
clinical phobias, the psy-chiatrist should consider the extent of the
individual’s avoidance, the frequency with which the phobic stimulus is
encountered, and the degree to which the individual is bothered by having the
fear. For example, an individual who fears seeing snakes in the wild but who
lives in the city never encounters snakes, and never even thinks about snakes
would probably not be diagnosed with a specific phobia. In contrast, when an
individual’s fear of snakes leads to avoidance of walking through parks,
camping, swim-ming and watching certain television programs, despite having an
interest in doing these things, a diagnosis of specific phobia would be
appropriate.
Similar factors should be considered in deciding at what point normal
shyness reaches an intensity that warrants a diag-nosis of social phobia. An
individual who is somewhat quiet in groups or when meeting new people but does
not avoid these situ-ations and is not especially distressed by his or her
shyness would probably not receive a diagnosis of social phobia. In contrast,
an individual who frequently refuses invitations to socialize because of
anxiety, quits a job because of anxiety about having to talk to customers, or
is distressed about her or his social anxiety would be likely to receive a
diagnosis of social phobia.
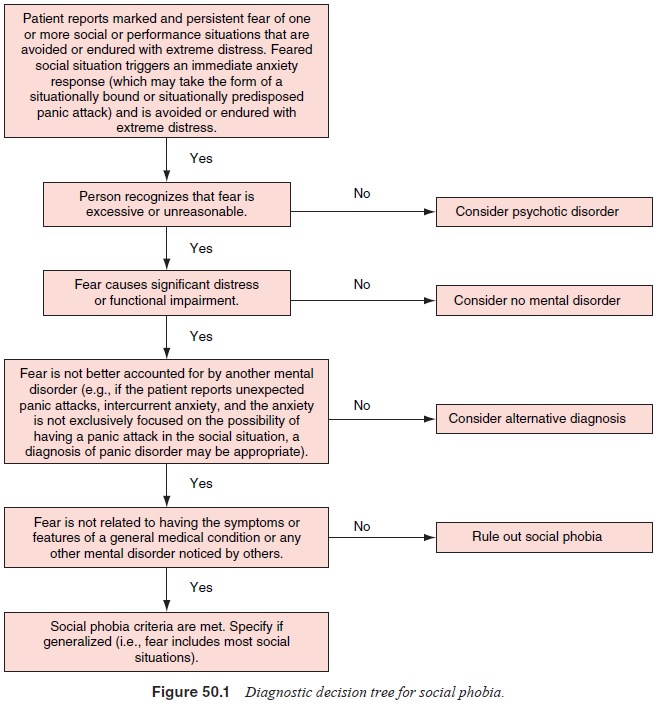
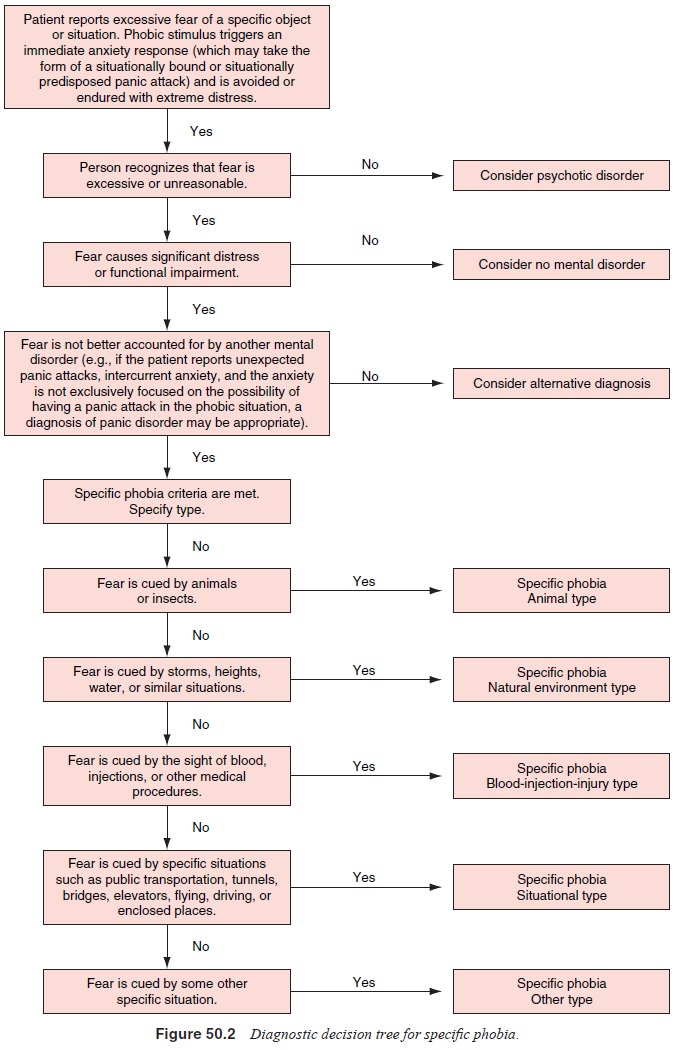
Diagnostic decision trees for social and specific phobias are presented
in Figures 50.1 and 50.2.
Related Topics