Chapter: Essentials of Psychiatry: Anxiety Disorders: Social and Specific Phobias
Social and Specific Phobias: Assessment
Assessment
Special Issues in Psychiatric Examination and History
During all parts of the initial evaluation, the psychiatrist should be
sensitive to several issues. First, for many patients with pho-bias, even
discussing the phobic object can provoke anxiety. For example, some patients
with spider phobias experience panic at-tacks when they discuss spiders. Some
patients with blood pho-bias faint when they discuss surgical procedures.
Therefore, the psychiatrist should ask the patient whether discussing the
phobic object or situation will provoke anxiety. If the interview is likely to
be a source of stress, the psychiatrist should emphasize the importance of the
information that is being collected, as well as the potential therapeutic value
of discussing the feared object. As described in a later section, exposure to
the feared stimulus is an essential component of the treatment of most specific
pho-bias. Of course, the interviewer should use his or her judgment when
deciding how much to push the patient in the first session. For treatment to be
effective, establishing trust in the psychiatrist early in the course of
treatment is essential.
With respect to social phobia, the assessment itself may be considered a
phobic stimulus. Because individuals with social phobia fear the evaluation of
others, a psychiatric interview may be especially frightening. Even completing
self-report question-naires in the waiting room may be difficult for patients
who fear writing in front of others. The psychiatrist should be sensitive to
this possibility and provide reassurance when appropriate.
Structured and Semistructured Interviews
Although there are numerous structured and semistructured in-terviews
available, two of the most commonly used interviews for diagnosing anxiety
disorders are the Anxiety Disorders In-terview Schedule for DSM-IV (ADIS-IV)
(Brown et al., 1994) and the
Structured Clinical Interview for Axis I DSM-IV-TR Disorders-Patient Edition
(SCID-I/P for DSM-IV-TR) (First et al.,
2001). Current and lifetime diagnoses of specific phobia and social phobia based on the ADIS-IV have been shown to have
good to excellent reliability for the specific phobia types and the generalized
type of social phobia. Each interview has advantages and disadvantages.
Although the SCID-I provides detailed assessment of a broader range of
disorders relative to the ADIS-IV (including eating disorders and psychotic
disor-ders), the ADIS-IV provides more detailed information on each of the
anxiety disorders and, like the SCID-I, includes sections to provide DSM-IV
diagnoses for the mood disorders and other disorders that are typically
associated with the anxiety disorders (e.g., substance use and somatoform
disorders). In addition, the ADIS-IV includes more questions to help
differentiate specific and social phobias from other disorders with which they
share features.
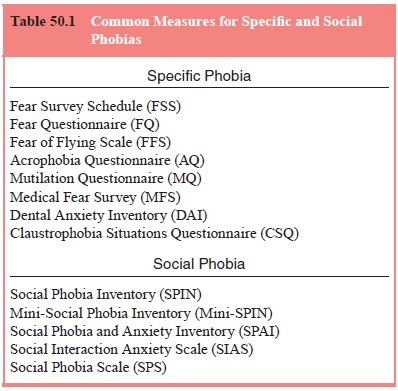
Self-report Measures
Numerous self-report measures have been created for the assess-ment of
specific phobias and social anxiety. The main advantage of self-report measures
is the time that they save for the psychia-trist. Relevant self-report measures
are recommended before the clinical interview if possible. This will allow the
interviewer to follow up specific responses during the interview. Measures can
be administered again, periodically, to assess progress and out-come. It should
be noted that questionnaire measures do not al-ways correlate highly with
performance on behavioral measures. Furthermore, there is evidence that men are
more likely than women to underestimate their fear on specific phobia measures.
The most common questionnaires used to screen for specific phobias are the
various versions of the Fear Survey Schedule. In addition, a variety of
measures exist to assess fear of specific objects and situations. For example,
the Mutilation Question-naire (Klorman et
al., 1974) is among the most common tests for assessing fear of situations
involving blood and medical pro-cedures. Self-report measures for assessing
both specific phobia and social anxiety are listed in Table 50.1.
Behavioral Tests
Behavioral testing is an important part of any comprehensive evaluation for a phobic disorder. This is particularly the case if behavioral or cognitive–behavioral treatment will be used. Because most individuals with phobias avoid the objects and situations that they fear, patients may find it difficult to describe the subtle cues that affect their fear in the situation. In addition, it is not unusual for patients to misjudge the amount of fear that they typically experience in the phobic situation. A behavioral approach test can be useful for identifying specific fear triggers as well as for assessing the intensity of the patient’s fear in the actual situation.
To conduct a behavioral approach test, patients should be instructed to
enter the phobic situation for several minutes. For example, an individual with
a snake phobia should be instructed to stand as close as possible to a live
snake and note the specific cues that affect the fear (e.g., size of snake,
color, movement) and the intensity of the fear (perhaps rating it on a
0–100-point scale). Patients should pay special attention to their physical
sensations (e.g., palpitations, sweating, blushing), negative thoughts (e.g.,
“I will fall from this balcony”) and anxious coping strategies (e.g., escape,
avoidance, distraction).
The behavioral approach test will help in the develop-ment of a specific
treatment plan. However, before treatment patients will often be reluctant to
enter the feared situation. If this is the case, the information collected
during the behavioral approach test may be elicited during the early part of
behavioral treatment.
Differences in Sex, Cultural and Developmental Presentation
Sex Differences
As mentioned earlier, specific phobias tend to be more common among
women than men. This finding seems to be strongest for phobias from the animal
type, whereas sex differences are smaller for height phobias and
blood-injury-injection phobias. In addition, social phobia tends to be slightly
more prevalent among women than men, although these differences are rela-tively
small.
There are several reasons why women may be more likely than men to
report specific phobias. First, men tend to underreport their fear. Also, women
may be more likely than men to seek treatment for their difficulties, which
would account for the fact that sex differences are often larger in treatment
samples compared with epidemiological samples. In addition sex ratios for
phobias differ across cultures, which may be explained by cultural differences
in treatment seeking. Finally, the sex differ-ence in prevalence may reflect
actual differences between men and women in susceptibility to develop phobias.
Women and men are taught to deal differently with typi-cal phobic
stimuli. Traditionally, boys more than girls are often encouraged to play with
spiders and toy snakes and to engage in more adventurous activities (e.g.,
hiking in high places). In ad-dition, women may have more role models for the
development of fear than do men. Images of women standing on chairs when they
see a mouse or running away from spiders are common in children’s cartoons and
other media, but men are rarely depicted as being frightened by these objects.
Therefore, it is possible that in Western cultures women learn to fear certain
situations more strongly than do men. Of course, it is difficult to know
whether culture and the media are responsible for sex differences or sim-ply
reflect differences that exist for other reasons (e.g., different predisposing
factors). It will be interesting to see whether sex ratios for phobias change
as traditional gender roles continue to change
Cultural Differences
Little is known about cultural differences in specific and social
phobias. Nevertheless, a few studies bear on the issue of cultural differences
in phobias. For example, there is evidence from epi-demiological studies that
African-Americans are 1.5 to 3 times as likely as whites to report phobic
disorders, even after controlling for education and socioeconomic status.
Several explanations for this finding have been provided. For example, some of
the fears reported by African-American individuals may reflect realistic
concerns that were misdiagnosed as phobias. For example, Afri-can-American
persons in inner city communities may have more realistic reasons to fear
violence. Furthermore, African-Ameri-cans experience more negative evaluation
from others, and some of their social concerns may be realistic. Another
possibility is that African-Americans experience more chronic stress than
whites and therefore may be more susceptible to the development of phobias and
other problems. Finally, there may be cultural dif-ferences in response biases
on questionnaire measures of fear and during interviews.
Research
has found that specific phobias, but not social phobias, are more common among
US-born Mexican-Americans than in US-born whites or immigrant
Mexican-Americans, after controlling for sex, age, socioeconomic status and
various other variables. A variety of studies have shown that specific phobias,
social phobia and related conditions exist across cultures. For ex-ample, in
Japan, a condition exists called taijin kyôfu in which in-dividuals have an “obsession of
shame”. This condition has much overlap with social phobia in that it is often
accompanied by fears of blushing, having improper facial expressions in the
presence of others, looking at others, shaking and perspiring in front of
others. In addition, studies have identified individuals with so-cial and
specific phobias in a variety of other nonWestern coun-tries including Saudi
Arabia, India, Japan and other East Asian countries. Interestingly, in some
other cultures, the sex ratio forphobias
tends to be reversed. For example, in studies from Saudi Arabia and India, up
to 80% of individuals reporting for treat-ment of phobias were male.
Psychiatrists treating patients from different cultures should be aware
of cultural differences in presentation and re-sponse to treatment, such as
cultural differences in verbal com-munication styles, proxemics (i.e., use of
interpersonal space), nonverbal communication and other verbal cues (e.g., tone
and loudness). Many cues that a psychiatrist might use to aid in the diagnosis
of social phobia in white Americans may not be use-ful for diagnosing the
condition in other cultures. For example, although many psychiatrists interpret
a lack of eye contact as indicating shyness or a lack of assertiveness,
avoidance of eye contact among Japanese and Mexican-Americans is often viewed
as a sign of respect. In contrast to white Americans, Japanese are apparently
more likely to view smiling as a sign of embar-rassment or discomfort.
Furthermore, cultural differences in tone and volume of speech may lead
psychiatrists to misinterpret their patients. For example, whereas white
Americans are often un-comfortable with silence in a conversation, British and
Arab in-dividuals may be more likely to use silence for privacy and other
cultures use silence to indicate agreement among the parties or a sign of
respect. In addition, Asian individuals have been reported to speak more
quietly than white Americans, who in turn speak more quietly than those from
Arab countries. Therefore, differ-ences in the volume of speech should not be
taken to imply differ-ences in assertiveness or other indicators of social
anxiety.
Treatment methods may have to be adapted for different cultures. For
example, the direct style of many cognitive and be-havioral therapists may be
more likely to be perceived as rude or insensitive by individuals with certain
cultural backgrounds than those with other backgrounds. It should be noted that
individu-als within a culture differ on these variables just as individuals
across cultures differ. Therefore, although psychiatrists should be aware of
cultural differences, these differences should not blind the psychiatrist to
relevant factors that are unique to each individual patient.
Developmental Differences
Among children, specific and social fears are common. Be-cause these
fears may be transient, DSM-IV-TR has included a provision that social and
specific phobias not be assigned in children unless they are present for more
than 6 months. In addition, children may be less likely than adults to
recognize that their phobia is excessive or unrealistic. The specific ob-jects
feared by children are often similar to those feared by adults, although
children may be more likely to fear objects and situations that are not easily
classified in the four main specific phobia types in DSM-IV-TR (e.g., balloons
or costumed char-acters). In addition, children often report specific and
social phobias having to do with school. Children with social phobia tend to
avoid changing for gym class in front of others, eating in the cafeteria, or
speaking in front of the class. They may stay home sick on days when
frightening situations arise or may make frequent trips to the school nurse.
Whereas some investigators have found that boys and girls are equally likely to
present for treatment of phobias, others have found social phobia to be more
common among girls. In one prospective study of childhood anxiety disorders,
Last and colleagues (1996) found that almost 70% of children with a specific
pho-bia were recovered over a 3- to 4-year period compared with arecovery rate
of 86% for social phobia. Thus, almost a third of the clinical sample with
specific phobia had symptoms that still met clinical criteria for specific
phobia at the end of the follow-up period. This was the lowest recovery rate
among the anxi-ety disorders that were studied. However, those in the clinical
sample with specific phobia had the lowest rate of development of new
psychiatric disorders (15%) compared with the other anxiety disorders studied
(e.g., the rate of development for new psychiatric disorders was 22% for those
in the clinical sample with social phobia).
Related Topics