Chapter: Clinical Dermatology: Sebaceous and sweat gland disorders
Rosacea
Rosacea
Rosacea
affects the face of adults, usually women. Although its peak incidence is in
the thirties and forties, it can also be seen in the young or old. It may
coexist with acne but is distinct from it.
Cause and histopathology
The
cause is still unknown. Rosacea is often seen in those who flush easily in
response to warmth, spicy food, alcohol or embarrassment. Any psychological
abnormalities, including neuroticism and depression, are secondary to the skin
condition. No pharmaco-logical defect has been found which explains these
flushing attacks. Sebum excretion rate and skin micro-biology are normal. A
pathogenic role for the hair fol-licle mite, Demodex folliculorum,
has not been proved.
Clinical course and complications
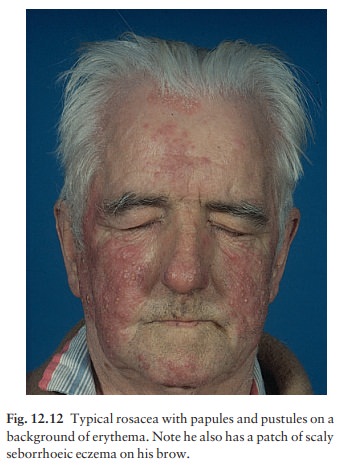
The
cheeks, nose, centre of forehead, and chin are most commonly affected; the
peri-orbital and peri-oral areas are spared (Fig. 12.12). Intermittent flushing
is followed by a fixed erythema and telangiectases. Discrete domed inflamed papules,
papulopustules and, rarely, nodules develop later. Rosacea, unlike acne, has no
comedones or seborrhoea. It is usually symmetrical. Its course is prolonged,
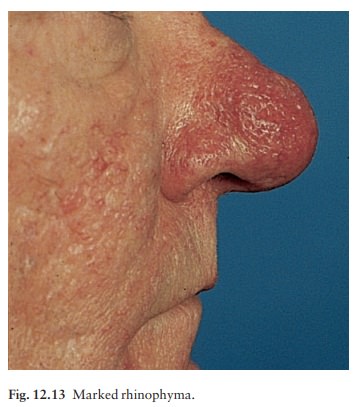
with exacer-bations and remissions. Complications include ble-pharitis,
conjunctivitis and, occasionally, keratitis. Rhinophyma, caused by hyperplasia
of the sebaceous glands and connective tissue on the nose, is a striking
complication (Fig. 12.13) that is more common in males. Lymphoedema, below the
eyes and on the fore-head, is a tiresome feature in a few cases. Some patients
treated with potent topical steroids develop a rebound flare of pustules, worse
than the original rosacea, when this treatment is stopped.
Differential diagnosis
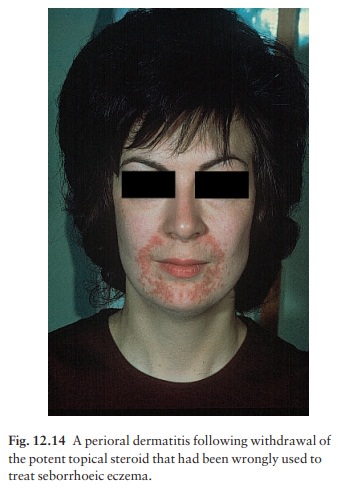
Acne
has already been mentioned. Rosacea differs from it by its background of
erythema and telangiec-tases, and by the absence of comedones. The distribu-tion
of the lesions is different too, as rosacea affects the central face but not
the trunk. Also rosacea usu-ally appears after adolescence. Seborrhoeic eczema,
perioral dermatitis (Fig. 12.14), systemic lupus ery-thematosus and photodermatitis should be considered, but
do not show the papulopustules of rosacea. The flushing of rosacea can be
confused with menopausal symptoms and, rarely, with the carcinoid syndrome.
Superior vena caval obstruction has occasionally been mistaken for lymphoedematous
rosacea.
Treatment
Tetracyclines, prescribed as for acne, are the traditional treatment and are usually effective. Erythromycin is the antibiotic of second choice. Courses should last for at least 10 weeks and, after gaining control with 500–1000 mg daily, the dosage can be cut to 250 mg daily.
The condition recurs in about half of the patients within 2
years, but repeated anti-biotic courses, rather than prolonged maintenance
ones, are generally recommended. Topical 0.75% metronidazole gel, applied
sparingly once daily, is nearly as effective as oral tetracycline and often
prolongs remission. It can be tried before systemic treatment and is especially
useful in treating ‘stuttering’ recurrent lesions that do not then need
repeated systemic courses of antibiotics. Rarely systemic metronidazole or
isotretinoin is needed for stubborn rosacea.
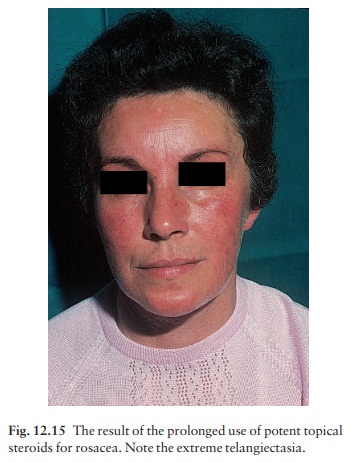
Rosacea and topical steroids go badly together (Fig. 12.15); if possible
patients should use traditional applications such as 2% sulphur in aqueous
cream or 1% ichthammol in zinc cream. Sunscreens may help if sun exposure is an
aggravating factor, but changes in diet or drinking habits are seldom of value.
Related Topics