Chapter: Clinical Dermatology: Sebaceous and sweat gland disorders
Acne Treatment
Treatment
Acne
frequently has marked psychological effects. Even those with mild acne need
sympathy. An optimistic approach is essential, and regular encouragement
worthwhile.
Occasionally
an underlying cause is found; this
should be removed or treated.
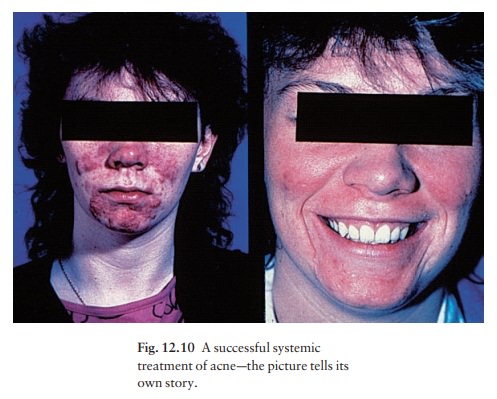
At
some time most teenagers try antiacne prepara-tions bought from their
pharmacist; local treatment is enough for most patients with comedo-papular
acne, although both local and systemic treatment are needed for pustulocystic
scarring acne (Fig. 12.10).
Local treatment
1
Regular gentle cleansing with soap
and water shouldbe encouraged, to remove surface sebum. Antibacterial cleansers
are also useful, e.g. chlorhexidine.
2 Benzoyl peroxide. This antibacterial agent isapplied only at night initially, but can be used twice daily if this does not cause too much dryness and irritation. It is most effective for inflammatory lesions It is wise to start with a 2.5 or 5% preparation, mov-ing up to 10% if necessary. Benzoyl peroxide bleaches coloured materials, particularly towels and flannels.
3 Retinoids. The
vitamin A (retinol) analogues(tretinoin, adapalene, tazarotene) normalize
follicular keratinization, and are especially effective against comedones.
Patients should be warned about skin irritation (start with small amounts) and
photosensit-ivity. Concomitant eczema is usually a contraindica-tion to its
use. Tretinoin can be prescribed as a lotion, cream or gel. New preparations
use microspheres (Retin-A micro) or specially formulated bases (Aveta) that
minimize irritation. The weakest preparation should be used first, and applied
overnight on altern-ate nights. Sometimes, after a week or two, it will have to
be stopped temporarily because of irritation. As with benzoyl peroxide, it may
be worth increasing the strength of tretinoin after 6 weeks if it has been well
tolerated. The combination of benzoyl peroxide in the morning and tretinoin at
night has many advocates.
•
Isotretinoin 0.05% is made up in a
gel base (not available in USA) and applied once or twice daily. It irritates
less than the same concentration of tretinoin.
•
Adapalene (0.1% gel) is a
retinoid-like drug indi-cated for mild to moderate acne. It appears to work
quicker and to be tolerated better than tretinoin.
•
Tazarotene (0.1% gel), applied once
daily, was found in one study to be more effective than tretinoin (0.1%
microsponge).
Topical
retinoids should not be prescribed for preg-nant woman with acne.
4 Azelaic acidis
bacteriocidal forP.
acnes: it isalso anti-inflammatory and inhibits the formation of
comedones by reducing the proliferation of ker-atinocytes. It should be applied
twice daily, but not used for more than 6 months at a time.
5 Abrasive
pastes containing aluminium oxide havelargely been replaced by
topical retinoids as aggress-ive scrubbing can rupture comedones.
6 Sulphur. A number
of time-honoured preparationscontaining sulphur are available on both sides of
the Atlantic. Some are included in Formulary 1.
7 Local antibiotics.
These include topical clindamy-cin, erythromycin and sulfacetamide.
8 Combinations. Some combinations work better thaneither of the drugs used separately. Erythromycin combined with a zinc acetate complex is popular and effective. It works as an antim-icrobial, an inhibitor of 5α-reductase , an antioxidant and as an immunomodulator. Ery-thromycin and clindamycin, in mixtures with benzoyl peroxide, reduce P. acnes numbers and the likeli-hood of resistant strains emerging.
9 Aluminium chloride.
Alcoholic solutions of alum-inium chloride, used as antiperspirants, may help
tropical acne.
10 Cosmetic camouflage.
Cover-ups help some pati-ents, especially females, whose scarring is unsightly.
They also obscure postinflammatory pigmentation. A range of make-ups is
available in the UK and USA.
Systemic treatment
Antibiotics: tetracyclines
• Oxytetracycline
and tetracycline. An averagestarting dosage for an adult is 250 mg up to
four times daily, but up to 1.5 g /day may be needed in resistant cases. The
antibiotic should not be used for less than 3 months and may be needed for a
year or two, or even longer. It should be taken on an empty stomach, 1 h before
meals, or 4 h after food, as the absorption of these tetracyclines is decreased
by milk, antacids and calcium, iron and magnesium salts. The dosage should be
tapered in line with clinical improvement, an average maintenance dosage being
250–500 mg / day. Even with long courses, serious side-effects are rare,
although candidal vulvovaginitis may force a change to a narrower spectrum
antibiotic such as erythromycin.
•
Minocycline, 50 mg twice daily or 100 mg once
ortwice daily (in a modified release preparation) is now preferred by many
dermatologists, although it is much more expensive. Absorption is not
significantly affected by food or drink. Minocycline is much more lipophilic
than oxytetracycline and so probably con-centrates better in the sebaceous
glands. It is bacterio-logically more effective than oxytetracycline and
tetracycline and, unlike erythromycin, little resistance to it by Proprionibacteria
has been recorded. It can be effective even when oxytetracycline has failed,
but can cause abnormalities of liver function and a lupus-like syndrome.
• Doxycycline, 100 mg once or twice daily is acheaper alternative to minocycline, but more fre-quently associated with phototoxic skin reactions.
Tetracyclines
should not be taken in pregnancy or by children under 12 years as they are
deposited in growing bone and developing teeth, causing stained teeth and
dental hypoplasia. Rarely, the long-term administration of minocycline causes a
greyish pigmentation, like a bruise, especially on the faces of those with
actinic damage and over the shins.
Erythromycin
(dosage as for oxytetracycline) isthe next antibiotic of
choice but is preferable to tetracyclines in women who might become pregnant.
Its major drawback is the development of resistant Proprionibacteria,
now present in at least one in fourpatients with acne, which leads to
therapeutic failure.
Trimethoprim
is used by some as a third-line anti-biotic for acne, when a
tetracycline and erythromycin have not helped. White blood cell counts should
be monitored. Ampicillin
is another alternative.
Hormonal.
A combined antiandrogen– oestrogentreatment (Dianette: 2 mg cyproterone acetate
and 0.035 mg ethinylestradiol) is available in many countries and may help
persistent acne in women. Monitoring is as for any patient on an oral
contracept-ive, and further contraceptive measures are unnecess-ary. Courses
last for 8–12 months and the drug is then replaced by a low oestrogen/low
progestogen oral contraceptive. These drugs are not for males.
A
triphasic pill, or a pill with a high oestrogen content, is best for women with
acne who also require oral contraception. Those on antibiotics should be warned
of their possible interaction with oral contra-ceptives and should use other
contraceptive precau-tions, especially if the antibiotics induce diarrhoea.
Isotretinoin
(13-cis-retinoic acid,).This is an oral
retinoid, which inhibits sebum excre-tion, the growth of P. acnes,
and acute inflammatory processes. The drug is reserved for severe nodulo-cystic
acne, unresponsive to the measures outlined above. It is routinely given for 4–
6 months only, in a dosage of 0.5–1 mg / kg body weight /day; young men with
truncal acne usually require the higher dosage. A full blood count, liver
function tests and fasting lipid levels should be checked, and routine urine
analysis performed before the start of the course, and then at 4 weeks after
starting the drug. Some physicians also monitor at 10 and 16 weeks and perform
a final check 1 month after completing the course. The drug seldom has to be
stopped, although rarely abnormalit-ies of liver function limit treatment.
Isotretinoin is highly teratogenic: before starting treatment women should sign a form confirming that, as far as they know, they are not pregnant and that they have been warned about this risk. They should take an oral contraceptive or Dianette for 2 months before starting isotretinoin, throughout treatment and for 1 month thereafter. Tests for pregnancy, prefer-ably performed on a blood sample, should be carried out twice before starting treatment and at follow-up visits. Contraception and teratogenicity of the drug must be discussed at all visits. The recommendations in the USA are especially stringent. Before receiving the drug the patient must sign that ‘I understand that I cannot receive a prescription for Accutane unless I have two negative pregnancy test results.
The first pregnancy test should be during the office visit when my prescriber
decides to prescribe Accutane. The sec-ond test should be on the second day of
my next men-strual cycle or 11 days after the last time I had unprotected
sexual intercourse, whichever is later. I understand that I will have
additional pregnancy testing, monthly, throughout my Accutane therapy.’
Furthermore, the manufacturer’s medication guide recommends that ‘you must use
two separate effective forms of birth control at the same time for at least 1
month before starting Accutane, while you take it, and for 1 month after you
stop taking it’. Treatment should start on day 3 of the patient’s next
menstrual cycle following a negative pregnancy test.
Depression,
sometimes leading to suicide, is a rare accompaniment of treatment. A causal
relationship seems likely in a few patients, although this has yet to be
confirmed in a large controlled study. Nevertheless, patients and their family
doctors should be warned about the appearance or worsening of depression before
starting a course of isotretinoin and patients should be asked to sign a
document that indicates that the issue of adverse psychiatric events has been
dis-cussed. The drug should be stopped immediately if there is any concern on
this score. The possibility of adverse psychiatric events should be discussed
at all visits. This potentially severe accompaniment of isotretinoin treatment
has to be balanced against its remarkable efficacy in severe acne. The lives of
most patients with conglobate acne have been transformed after successful
treatment with isotretinoin.
Other
side-effects of isotretinoin include a dry skin, dry and inflamed lips and
eyes, nosebleeds, facial ery-thema, muscle aches, hyperlipidaemia and hair loss;
these are reversible and often tolerable, especially if the acne is doing well.
Rarer and potentially more serious side-effects include changes in night-time
vision and hearing loss. Occasionally, isotretinoin flares acne at first, but
this effect is usually short lived and the drug can be continued. It is because
of its early side-effects that some dermatologists start isotretinoin in a low
dose (e.g. 20 mg/day) and then work up to the target dose if no significant
side-effects are reported at review during the first month of treatment. Early
review appointments (e.g. at 1 and 2 weeks into treatment) are comforting to
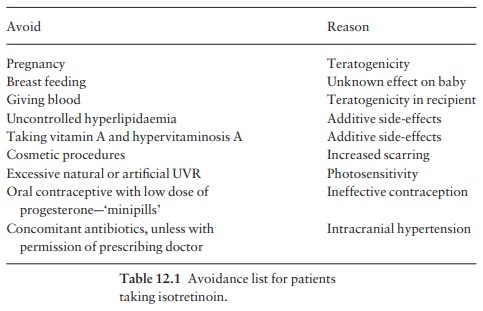
both patient and doctor. A useful ‘avoidance list’ for patients taking
isotretinoin is given in Table 12.1.
Diet
It
is sensible for patients to avoid foods (e.g. nuts, chocolates, dairy products
and wine) that they think make their acne worse, but there is little evidence
that any dietary constituent, except iodine, causes acne.
Physical
Ultraviolet
B radiation therapy often helps with exacer-bations. Two-month courses,
during which the patient attends two or three times weekly, are usually
adequate.
Cysts can
be incised and drained with or without alocal anaesthetic.
Intralesional injections of 0.1 mL of triamcinoloneacetonide (2.5 –10 mg /mL) hasten the resolution of stubborn cysts, but can leave atrophy.
Dermabrasion.
This helps to smooth out facial scars.A high-speed rotating wire brush planes
down to a bleeding dermis. Dermabrasion should not be carried out if there are
any active lesions and does not help depressed ‘ice-pick’ scars, which may best
be excised. Unsightly hyperpigmentation may follow in darker skins.
Microdermabrasion is well tolerated but its effects are usually transient.
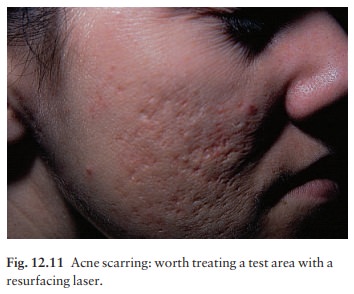
Lasers.
Skin resurfacing with CO2and erbium
lasersis rapidly replacing dermabrasion and chemical peel-ing as the best
treatment for postacne scarring. The procedure, which should be delayed until
the acne is quiescent, is usually performed under local anaesthe-sia. Initially
a small test area is treated and then assessed (Fig. 12.11). If the result is
satisfactory, the treatment is extended. In expert hands the results can be
dramatic.
Collagen
injections. Bovine collagen can be injectedinto depressed scars to
improve their appearance. Patients with a history of any autoimmune disorder
are excluded from this treatment. Shallow atrophic lesions do better than
discrete ‘ice-pick’ scars. The procedure is expensive and has to be repeated every
6 months as the collagen is resorbed.
Related Topics