Chapter: Clinical Dermatology: Sebaceous and sweat gland disorders
Eccrine sweat glands
Sweat
glands
Eccrine
sweat glands
There
are 2 –3 million sweat glands distributed all over the body surface but they
are most numerous on the palms, soles and axillae. The tightly coiled glands lie
deep in the dermis, and the emerging duct passes to the surface by penetrating
the epidermis in a corkscrew fashion. Sweat is formed in the coiled gland by
active secretion, involving the sodium pump. Some damage occurs to the membrane
of the secret-ory cells during sweating. Initially sweat is isotonic with
plasma but, under normal conditions, it becomes hypotonic by the time it is
discharged at the surface, after the tubular resorption of electrolytes and
water under the influence of aldosterone and antidiuretic hormone.
In
some ways the eccrine sweat duct is like a renal tubule. The pH of sweat is
between 4.0 and 6.8; it contains sodium, potassium chloride, lactate, urea and
ammonia. The concentration of sodium chloride in sweat is increased in cystic
fibrosis, and sweat can be analysed when this is suspected.
Sweat
glands have an important role in temperature control, the skin surface being
cooled by evaporation. Up to 10 L/day of sweat can be excreted. Three stim-uli
induce sweating.
1 Thermal
sweating is a reflex response to a raisedenvironmental temperature
and occurs all over the body, especially the chest, back, forehead, scalp and
axillae.
2 Emotional sweatingis
provoked by fear or anxietyand is seen mainly on the palms, soles and axillae.
3 Gustatory sweatingis
provoked by hot spicy foodsand affects the face.
The
eccrine sweat glands are innervated by cholinergic fibres of the sympathetic
nervous system. Sweating can therefore be induced by cholinergic, and blocked
by anticholinergic drugs. Central control of sweating resides in the preoptic
hypothalamic sweat centre.
Clinical
disorders can follow increased or decreased sweating, or blockage of sweat
gland ducts.
Generalized hyperhidrosis
Thermal hyperhidrosis
The
‘thermostat’ for sweating lies in the preoptic area of the hypothalamus.
Sweating follows any rise in body temperature, whether this is caused by
exercise, environmental heat or an illness. The sweating in acute infections,
and in some chronic illnesses (e.g. Hodgkin’s disease), may be a result of a
lowering of the ‘set’ of this thermostat.
Other causes of general hyperhidrosis
•
Emotional stimuli, hypoglycaemia,
opiate with-drawal, and shock cause sweating by a direct or reflex stimulation
of the sympathetic system at hypothalamic or higher centres. Sweating
accompanied by a general sympathetic discharge occurs on a cold pale skin.
•
Lesions of the central nervous
system (e.g. a cerebral tumour or cerebrovascular accident) can cause
gener-alized sweating, presumably by interfering directly with the hypothalamic
centre.
• Phaeochromocytoma, the carcinoid syndrome, dia-betes mellitus, thyrotoxicosis, Cushing’s syndrome and the hot flushes of menopausal women have all been associated with general sweating. The mechan-isms are not clear.
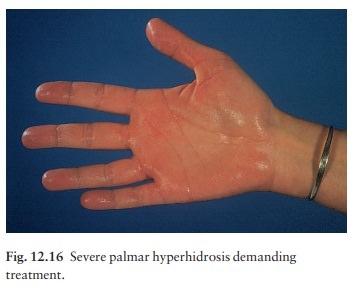
Local hyperhidrosis (Fig.
12.16)
Local hyperhidrosis plagues many young adults. The most common areas to be affected are the palms, soles and axillae. Too much sweating there is embarrassing, if not socially crippling.
A sodden shirt in contact with a dripping armpit, a wet
handshake and stinking feet are hard crosses to bear. Seldom is any cause
found, but organic disease, especially thyrotoxicosis, acromegaly, tuberculosis
and Hodgkin’s disease should be considered. A blatant anxiety state is
occasionally present, but more often an otherwise normal person is
understandably concerned about his or her antisocial condition. A vicious
circle emerges, in which increased anxiety drives further sweating.
These
problems may be no more than one end of the normal physiological range. How
many students sitting examinations have to dry their hands before putting pen
to paper? It is only when the sweating is gross, or continuous, that medical
advice is sought. Such sweating is often precipitated by emotional stimuli and
stops during sleep.
Treatment
Topical
applications. The most useful preparation foraxillary hyperhidrosis is
20% aluminium chloride hexahydrate in an alcohol base. At first it is applied
to the dry axillae every night. Soon the interval can be increased, and many
need the preparation only once or twice a week. The frequency may have to be
cut down if the preparation irritates the skin, which is most likely if it is
applied after shav-ing or when the skin is wet. Aluminium chloride also helps
hyperhidrosis of the palms and soles, but it is less effective there.
Potassium
permanganate soaks (1 : 10 000 aqueous solution) combat the bacterial
superinfection of sweaty feet that is responsible for their foul smell.
Patients should soak their feet for 15 min twice a day until the smell has
improved and be warned that potassium permanganate stains the skin and
everything else brown. Occasionally glutaraldehyde solutions are used instead,
but allergy and yellow-stained skin are potential com-plications. Topical
clindamycin is also effective.
Iontophoresis.
This is the passage of a low-voltagedirect current across
the skin. Iontophoresis with tap water or with the anticholinergic drug
glycopyrro-nium bromide (glycopyrolate, USA) may help palmar or plantar
hyperhidrosis. Patients attend two or three times a week for treatment until
the condition improves. Repeated courses or maintenance therapy may be
required.
Botulinum
toxin. This binds to presynaptic nervemembranes and then inhibits
the release of acetyl-choline. It is now the treatment of choice for severe
axillary or plantar hyperhidrosis, unresponsive to medical measures. Subdermal
aliquots of the toxin are injected into the hyperhidrotic area of the axilla or
sole, one region at a single session. Sweating is abolished after a delay of
2–3 days. Repeat injections (about every eighth month) are necessary as the
sweating returns when the toxin has gone. Antibodies may form against the toxin
and diminish its long-term effectiveness. Botulinum toxin is used less often
for palmar hyperhidrosis because of the risk of paralys-ing the intrinsic
muscles of the hand.
Systemic
treatment. Oral anticholinergic agents suchas Pro-Banthine and
glycopyronium bromide (USA) are sometimes tried but their side-effects limit
their value.
Surgery.
This is used less nowadays as the abovemeasures are usually effective. However,
recalcitrant axillary hyperhidrosis can be treated by removing the vault of the
axilla, which bears most of the sweat glands. These can be identified
preoperatively by apply-ing starch and iodine, which interact with sweat to
colour the sweat gland openings blue. Thoracoscopic sympathetic trunkotomy
(between the first and sec-ond thoracic ganglia) is effective for severe palmar
hyperhidrosis alone but is a last resort.
Hypohidrosis and anhidrosis
Anhidrosis caused by abnormality of the sweat glands
Heat
stroke. Caused by sweat gland exhaustion, thisis a medical
emergency seen most often in elderly
people
moving to a hot climate. It can also occur in the young, during or after
prolonged exercise, especially in hot climates. Patients present with
hyperthermia, dry skin, weakness, headache, cramps and confusion, leading to
vomiting, hypotension, oliguria, metabolic acidosis, hyperkalaemia, delirium
and death. They should be cooled down immediately with cold water, and fluids
and electrolytes must be replaced.
Hypohidrotic
ectodermal dysplasia. This rare disor-der is inherited
as an X-linked recessive trait, in which the sweat glands are either absent or
decreased. Affected boys have a characteristic facial appearance, with poor
hair and teeth (Figs 13.13 and 13.14), and are intolerant of heat.
Prematurity.
The sweat glands function poorly inpremature babies nursed in incubators and
hot nurseries.
Anhidrosis caused by abnormalities of the nervous system
Anhidrosis
may follow abnormalities anywhere in the sympathetic system, from the
hypothalamus to the peripheral nerves. It can therefore be a feature of multiple
sclerosis, a cerebral tumour, trauma, Horner’s syndrome or peripheral
neuropathy (e.g. leprosy, alcoholic neuropathy and diabetes). Patients with
widespread anhidrosis are heat-intolerant, develop-ing nausea, dizziness,
tachycardia and hyperthermia in hot surroundings.
Anhidrosis or hypohidrosis caused by skin disease
Local
hypohidrosis has been reported in many skin diseases, especially those that
scar (e.g. lupus erythe-matosus and morphoea). It may be a feature of Sjogren’s
syndrome, ichthyosis, psoriasis and miliaria profunda .
Interference with sweat delivery
Miliaria.
This is the result of plugging or rupture ofsweat ducts. It occurs in hot humid
climates, at any age, and is common in over-clothed infants in hot nurseries.
The physical signs depend on where the ducts are blocked.
Miliaria
crystallina. This presents as tiny clear non-inflamed vesicles that
look like dew. This is the most superficial type.
Miliaria
rubra (prickly heat). Tiny erythematous andvery itchy papules.
Miliaria
profunda. These consist of larger erythema-tous papules or pustules.
This is the deepest type.
Treatment.
The best treatment is to move to a coolerclimate or into air conditioning.
Clothing that pre-vents the evaporation of sweat (e.g. nylon shirts) should be
avoided; cotton is best. Claims have been made for ascorbic acid by mouth, but
in our hands it rarely if ever helps. Topical steroids reduce irritation but
should only be used briefly. Calamine lotion cools and soothes.
Related Topics