Chapter: Medicine Study Notes : Emergency Management
Resuscitation Ethics - Resuscitation Emergency Management
Resuscitation Ethics
CPR Efficacy
·
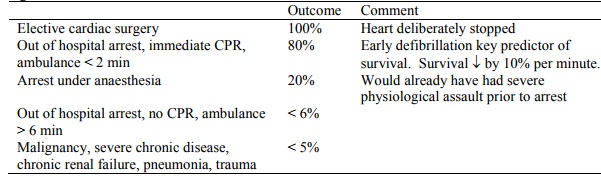
Wide variation in outcome
depending on clinical circumstances. Discharge rate is 15%. Biased by large
number of „futile‟ resuscitations.
·
Poor outcomes (e.g. brain damage,
organ failure) are inversely correlated with chances of survival.
·
Age per se is not an independent
predictor of survival after CPR – but is correlated with illness
CPR and Consent
·
Family members are not able to give
consent (either for treatment or withdrawal treatment) under common law in NZ,
although H&DC Code has provision for taking into account “the views of
other suitable persons who are interested in the welfare of the consumer…”
·
Doctor must make a „substituted
professional judgement‟: immediate decision on available information (usually
not much) of what is in the patient‟s best interests
·
Ethically wrong to undertake
resuscitation in patients in whom it is possible to predict a very low rate of
intact survival
·
Futile treatment diverts
resources from other people. It is the principle of justice not the principle
of autonomy that creates a right to treatment
·
Doctor‟s should not make
decisions based on their assessment of the patient‟s quality of life. Only the
patient can make this assessment. However, this information is not usually
available in acute setting. Revise further resuscitation/treatment decisions
when this becomes available (i.e. the decision to resuscitate or not is not
static)
·
There is no ethical difference
(may be other differences) between withholding and withdrawing treatment. Can
revise decision to resuscitate as the probability of poor outcome grows or
other information (e.g. patient‟s wishes) comes to light
DNR Orders
·
= Do not resuscitate, DNAR = Do
not attempt resuscitation
·
Reasons for DNR orders:
o Refusal by a competent and informed patient
o Poor quality of life after CPR (patient‟s, not doctor‟s view)
o Futility: a clinical decision – so should the patient be involved or
not?
·
DNR orders should be discussed
where:
o Requested by a competent patient
o Considered on grounds of poor quality of life
·
Circumstances where it is not
necessary to discuss DNR orders:
o Patient is incompetent
o Competent patient but grounds of quantitative futility
o Where discussion of CPR would be detrimental to patient‟s well being
o Where patient indicates they do not wish to discuss CPR
·
Role of family/friends: get their
input, but doctor makes the decision regarding CPR unless the patient has a
welfare guardian or has an advance directive
·
Other points:
o A DNR doesn‟t mean other treatment is withdrawn
o DNRs must be clearly documented in notes, including discussion of decision making process
o DNRs should be reviewed regularly and may be withdrawn if warranted by
change in clinical circumstances
Related Topics