Chapter: Medicine Study Notes : Emergency Management
Cardiopulmonary Resuscitation (CPR) - Resuscitation Emergency Management
Emergency Management
Resuscitation
·
Objective: keep oxygenated blood
flowing to the brain – otherwise cell death in 2 – 4 minutes
·
Basic life support = no special
equipment
·
Advanced life support = basic
support + equipment + drugs
·
Early defibrillation is vital:
increasingly non-doctors are being trained to use it outside hospital setting
Cardiopulmonary
Resuscitation (CPR)
Summary
·
Ensure safety
·
Check responsiveness
·
Send for help
·
Open Airway
·
Check breathing/circulation: no
longer than 20 seconds
·
Precordial thump (if arrest
within last 90 secs)
·
Go for help
· 2 Effective Breaths – up to 5 attempts
· Chest compression/ventilation: adult 2 breaths per 15 compressions at 100 bpm, neonates 1 breath per 5 compressions 100 bpm
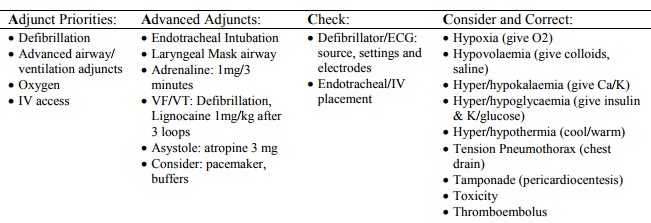
· ASAP: attach monitor Defibrillator and assess rhythm
·
VF or VT or AED „shock advised‟:
o Defibrillate: 200, 200, 360J (3 * 360J thereafter)
o Adrenaline every 3 minutes
o I minute CPR
·
Not VF or VT or No Shock Advised
o Adrenaline
o 3 minutes CPR
·
Reassess rhythm or circulation
A – Approach, Assess, Airway
·
Ensure own safety, summon help
·
Assess for responsiveness (gently
shake, shout, be careful of other injuries). An arrest may present as a short
grand mal seizure
·
Cervical spin injury should be
suspected, and assumed in unconscious patient esp. trauma. However, airway
management takes precedence
·
Urgent airway support may be
indicated by: respiratory distress, hypoventilation, absent response to pain or
stimuli, major skull, face or neck trauma, chest injuries, high spinal cord
injury
·
Open airway: CNS depression will
diminish muscle tone in upper airway ® tongue and epiglottis will
obstruct airway ® further hypoxia (faster in kids due to higher metabolic rate)
·
Tilt head back, chin lift, jaw
thrust
Airway Management Techniques
·
Oropharyngeal airway insertion:
o To maintain airway or prevent biting
o Use Geudal airway. Male size 4,
female size 3
o If they tolerate oropharyngeal airway without gagging or coughing Þ no protective reflexes and need to be endotracheally intubated as soon as practical to protect from aspiration
·
Laryngeal mask insertion:
o For failed endotracheal intubation where Positive Pressure Ventilation
indicated
o Doesn‟t protect from aspiration
o Male size 4, female size 3
· Endotracheal intubation:
o For control of airway, ventilation, protection from aspiration and
prevention of gastric distension (e.g. in bag mask ventilation)
o Sizes: Adult male size 9, female size 8, child (age in years)/4 + 4
o If conscious and struggling may require sedative (e.g. thiopentone) and
relaxant (suxamethonium)
o Always check chest movements and CO2 return to check you haven‟t got it
in the oesophagus
o Watch for pressure necrosis of tracheal mucosa from too large a tube or inflation
o Never attach O2 directly to tube (® over inflation) – always via a
ventilation/bag mask system
·
Bag mask ventilation (AMBU Bag)
o Always check chest rising: watch for leaks around mask, check patent airway
o Too much pressure ® gastric distension and aspiration into unprotected trachea
·
Cricothyrotomy:
o Use to gain access to airway where other methods have failed
o Clean skin with antiseptic solution
o Find cricothyroid membrane, between thyroid cartilage and cricoid ring immediately below it
o Make horizontal incision through membrane. Insert handle of scalpel into incision and rotate 90 degrees
o Insert largest possible endotracheal tube and attach to ambu bag. Ventilate with O2
o Alternatively, use size 14 cannula, at angle of 45 degrees pointing down
towards lungs. Attach cannula to syringe and syringe to ambu-bag
B – Breathing
· Ear over mouth and nose and look for chest to rise and fall. Slow gasping respirations may persist after arrest but these are ineffectual
·
Assess whether trachea central,
breath sounds bilateral, and check for crepitus (®
?pneumothorax)
·
Exclude life threatening chest
injuries: tension or open pneumothorax, flail segment
C – Circulation
·
Check carotid pulse.
·
Look for signs of circulation:
movement, colour, etc
Action Plan
· If breathing and circulation but unconscious ® recovery position, and maintain airway
· If not breathing but there is circulation ® ventilate with 10 expired air ventilations over a minute and reassess
·
If chest moving but there is no
flow of air then obstruction ® head tilt, chin lift, jaw thrust forward
·
If breathing absent or
deteriorating and no or unsure of circulation then presume arrest
· Commence CPR/defibrillation, but consider (if you can):
o Use O2 if at all possible – they will be hypoxic. Cylinders are black with white shoulder. Connect to ventilation bag at 4 atm. or to mask if breathing spontaneously (minimum 4 – 5 L per minute). NEVER connect directly to endotracheal tube (would ® barotrauma)
o Gaining iv access e.g. antecubital vein. Give saline flush after each access and hold limb up
o (circulation will be sluggish). Nothing more distal on arm, and don‟t
use femoral (unless needed for fluid replacement in trauma). If can‟t get
access, use carotid (subclavian interferes with CPR), or down endotracheal tube
(2 to 2.5 times iv dose) with 10 ml saline
Adult CPR
·
If defibrillator available,
consider immediate use
·
If no defibrillator and arrest
has occurred within 90 – 120 seconds then single precordial thump – may convert
ventricular arrhythmias in small number of cases, should never break bones,
never in presence of palpable pulse (as may cause VF if delivered on T wave –
commotio cordis)
·
Get help: it is most likely a VF
(and other things have a poor prognosis) and you need to defibrillate
· Continue with cycles of:
·
2 expired air ventilations (mouth
to mouth or nose, normal not big breath otherwise inflate stomach ® gastric
reflux, allow time for expiration). Theoretical risk of infection ® take
precautions
·
15 chest compressions:
·
Raise legs ® venous
return
·
Press over junction of middle and
lower thirds of sternum · Use only heel of hand with thumb side lower
·
Lock elbows, push straight down,
move from hips not shoulders. Get on bed
if you‟re too low
· Consider putting board under patient or place on floor – soft mattress will impair compression · Depress 4-5cm or one third of chest thickness: it is depth not force that is important, equal
§ compression and relaxation times, not too jerky. Start gentle to
determine correct pressure. Rib fractures impede filling, cause pneumothorax,
lacerations of liver and spleen, and fat emboli
·
Rate of 100 per minute for adults
and children.
·
Can achieve systolic pressure of
60 – 80 mmHg, but low diastolic pressure so brain perfusion maintained but
heart perfusion poor. Adrenaline improves diastolic pressure
·
If two operator, still use 2:15
breaths per compressions. If patient not intubated pause 1 sec for ventilation.
No pause necessary if intubated
·
After 3 minutes, stop for 10 secs
to assess circulation. Continue with assessments every 3 minutes until
defibrillator arrives
·
Administer adrenaline 1 mg iv
with every 3 minute loop
Paediatric CPR
·
Respiratory distress/failure much
more common cause of cardiac arrest than cardiac problems. Hypoxia and global
ischaemia therefore often precede arrest (in adults it follows arrest), which
results in asystole – not VF. Also caused by hypovolaemia, poisoning, drowning,
etc
·
Ventilation therefore more
important than defibrillation. Kids have a higher metabolic rate and O2
reserves consumed quicker
·
Survival associated with duration
of arrest (after 5 minutes it plummets), not more than one dose of adrenaline,
and presence of VF
·
Procedure:
o Ensure your and patient‟s safety
o Assess responsiveness. Don‟t shake a baby. If unresponsive, shout for help
o Open airway: head tilt (not too much extension) and chin lift. Jaw
thrust instead if cervical trauma. Check for obstruction
o Assess breathing. If chest moves but no breath, recheck airway
o Ventilate: 5 attempted breaths 1 – 1.5 seconds. In babies and infants, give through nose or nose and mouth. Slow breaths at low pressure better than fast/high pressure (¯gastric distension). Ventilate just sufficiently to make chest rise and fall
o For no more than 10 secs, check circulation. Infants: brachial, femoral, axillary arteries or apex beat. If over 8, carotid best
o If no circulation or less than 60 bpm, external chest compression. Over
junction of middle and lower 3rd of sternum.
§ In neonates, use two fingers to depth of 1 – 1.5 cm. Rate of 100 bpm,
ratio of compressions to ventilations is 5:1
§ Kids over 5, heel of one hand, depth approx. 2 – 3 cm
§ Larger kids, two handed compression, depth of 3 – 4 cm, rate of 80 – 100 bpm, and ratio of 15: 2
o After one minute alert emergency services
o Resume CPR: reassess circulation after 3 minutes. Give adrenaline. If iv access time consuming, then 18 gauge perpendicular into anterior surface of tibia, 1 – 3 cm below tibial tuberosity. Failing this, give 10 times iv dose down endotracheal tube. Repeat cycle and adrenaline
o When defibrillator arrives, assess rhythm. Use paediatric paddles if
< 10 kg. ONLY if rhythm is VF or VT deliver 3 shocks at 2, 2, then 4 joules
per Kg. Perform CPR for one minute, reassess rhythm. Every 2nd loop give adrenaline
·
Ventilation: Harder in kids – use
two people to do bag-mask. Beware of
barotrauma
·
If hypovolaemia ® 20 ml/kg
saline or Ringers
Defibrillation
·
Produces a simultaneous
depolarisation of myocardial fibres ® allows coherent rhythm
·
Ideally within 90 seconds,
preferably within 8 minutes. DON‟T delay
defibrillation to allow period of
·
CPR
·
Apply ECG monitor
·
Switch on defibrillator (do this
in transit)
·
Check its NOT in synchronised
(cardioversion) mode
·
One paddle (doesn‟t matter which)
to right of upper sternum below the clavicle
· Other paddle just to the left of the normal apex beat
·
Use a conducting aid (either
electrode gel or pads), wipe up any gel that may short circuit between the pads
·
First, use paddles to assess
rhythm (check settings on defibrillator).
Classify as:
· Ventricular fibrillation or ventricular tachycardia (wide QRS complex):
o Charge defibrillator to 200J (for kids 2J/kg). This is low, but will
charge quicker and do less damage to myocardium
o „Stand clear‟: make sure you‟re not touching patient or bed
o Recharge defibrillator
o Observe ECG
o If VT or VF persists, deliver a second 200J shock, then 360J
o If VT/VF persists, 1 minute of CPR (attach ECG leads during this, insert
artificial airway, iv access etc)
o Repeat sequence, but with 360, 360, 360 then 1 minute CPR
o Adrenaline, 1 mg, with every 2nd loop (i.e. every 3 minutes)
o If following a shock an organised rhythm appears which could be associated with cardiac output, check circulation. If absent then 3 minutes of CPR
o If following a shock, the rhythm changes from VF/VT to asystole, perform
1 minute CPR and assess with NO adrenaline. „Stunned myocardium‟ may take 20 –
30 secs to start again
· Another rhythm. If asystole or electromechanical dissociation (if normal complex) then continue CPR in 3 minute loops, 1mg adrenaline per loop. Prognosis poor but consider:
o If asystole, is there an electrical fault, low gain on ECG. If in doubt deliver 3 defibrillating shocks
o If asystole with P waves (ventricular standstill) consider emergency transcutaneous electrical pacing
o Atropine, 3 mg iv, provides complete vagal blockade, as profound bradycardia may result from intense vagal over activity
o Treatment of precipitating condition
Cardioversion
·
Is timed via ECG to occur on the
R wave – must avoid the T wave (otherwise can ® VF)
·
Is used for:
o Ventricular tachycardia where pulse is present,
o Supraventricular dysrhythmias (SVT, atrial fibrillation, atrial flutter)
·
Won‟t fire unless it can detect
the QRS. So if trying to defibrillate and it‟s not working – check
defibrillator is not set to cardioversion
Related Topics