Chapter: Obstetrics and Gynecology: Reproductive Cycles
Reproductive Cycle
REPRODUCTIVE CYCLE
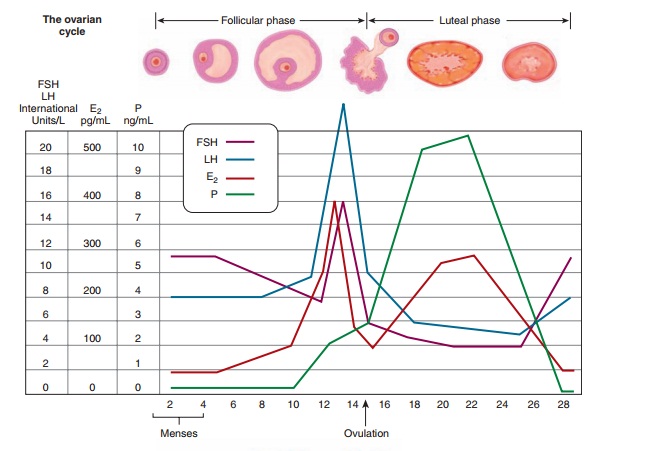
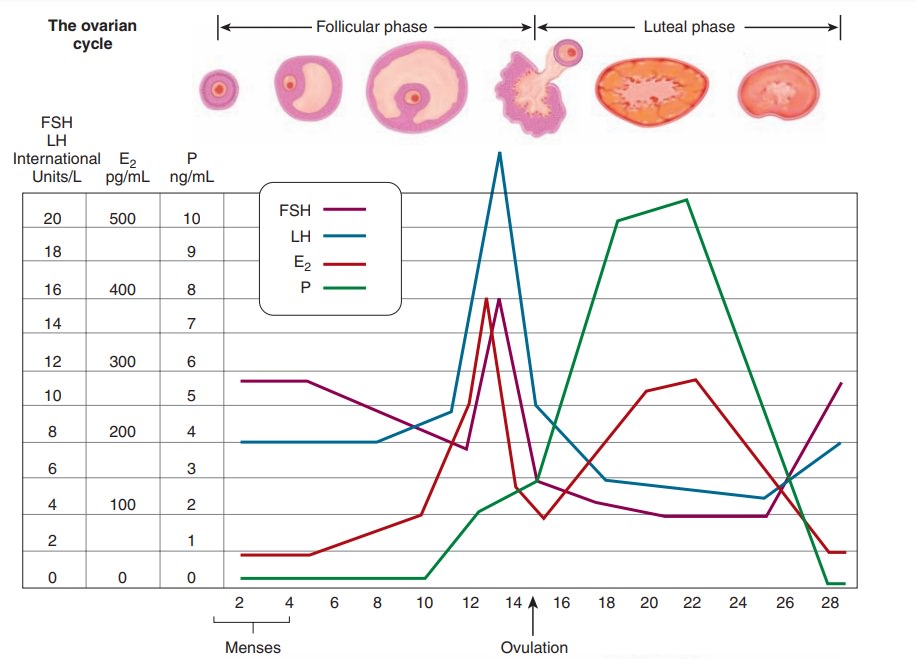
As discussed, the reproductive
cycle is divided into three phases: menstruation and the follicular phase,
ovulation, and the luteal phase. These three phases refer to the status of the
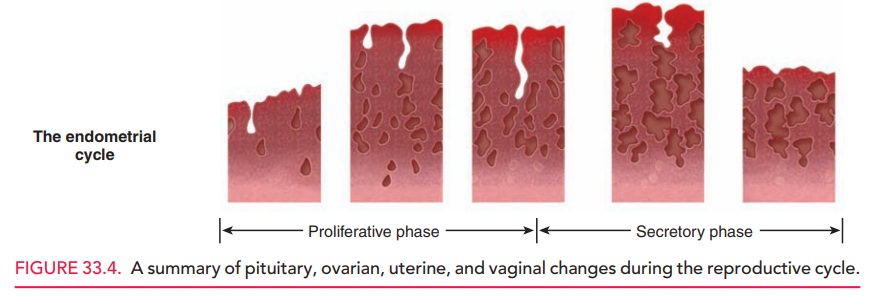
ovary during the reproductive cycle. In contrast, whenreferring to the endometrium, the phases of the menstrual cycle are
termed the proliferative and secretory phases.
Phase I: Menstruation and the Follicular Phase
The first day of menstrual bleeding is considered day 1 of the men-strual cycle. When conception does not occur, the involutionof the corpus luteum and, hence, the decline of proges-terone and estrogen levels cause menstruation. Normal menstruation lasts 3 to 7 days, during which women lose 20 to 60 mL of dark, nonclotting blood. Menstruation consists of blood and desquamated superficial endometrial tissues. Prostaglandins in the secretory endometrium and men-strual blood produce contractions of the uterine vasculature and musculature, which in turn cause endometrial ischemia and uterine cramping. These prostaglandin-associated uterine contractions also aid expulsion of the menstrual blood and tissue. Rising estrogen levels in the early follicu-lar phase induce endometrial healing which leads to cessa-tion of menstruation.
At the end of the luteal phase,
serum concentrations of estradiol, progesterone, and LH reach their lowest lev-els.
In response to low hormone levels, FSH begins to rise in the late luteal phase
before the onset of menstruation to recruit the next cohort of follicles. Thus, during menstrua-tion, follicular
growth has already been initiated for the new reproductive cycle. Estradiol
levels rise during the follicularphase, causing a decline in FSH. LH remains
low in the early follicular phase, but increasing estrogen levels have positive
feedback on LH release, and LH starts to rise by the midfollicular phase. Although
several follicles begin the maturation process, only the follicle with the
greatest number of granulosa cells and FSH receptors and the highest estradiol
production becomes the dominant folli-cle; the nondominant follicles undergo
atresia.
Phase II: Ovulation
As the dominant follicle secretes
an increasing amount of estradiol, there is marked positive feedback to the
pituitary gland to secrete LH. By days 11 to 13 of the cycle, the LH surge
occurs, which triggers ovulation. The LH surge begins 34 to 36 hours prior to
ovulation, and peak LH secretion occurs 10 to 12 hours prior to ovulation. With
the LH surge, the granulosa and theca cells undergo distinct changes and begin
production of progesterone. Meiosis of the primary follicle resumes after the LH
surge and the first polar body is released; the oocyte then arrests in
metaphase of the second meiotic division until fertilization occurs.
During ovulation, the oocyte is
expelled from the follicle, and the follicle is converted into the corpus
luteum.
Some women experience a twinge of
pain (“mittel-schmerz”) at the time
of ovulation and can precisely iden-tify the time of ovulation. Other women do
not experience this brief discomfort, but can recognize characteristic symptoms
that occur due to progesterone production after ovulation.
Phase III: Luteal Phase
The
luteal phase of the menstrual cycle is characterized by an alteration in the
balance of sex steroid secretion from predomi-nance of estrogen to predominance
of progesterone. The processof follicular
development has led to increased numbers of LH receptors on the granulosa and
theca cells. The mid-cycle LH surge stimulates these LH receptors and converts
the enzymatic machinery of these cells to produce and secrete progesterone;
this process is called luteinization.
Progesterone has negative feedback on pituitary secretion of FSH and LH, thus
both hormones are suppressed dur-ing the luteal phase. The corpus luteum also
produces estradiol in a pattern that parallels progesterone secretion.
The production of progesterone
begins approximately 24 hours before ovulation and rises rapidly thereafter.
Maximal progesterone production occurs 3 to 4 days after ovulation. The
lifespan of the corpus luteum ends approx-imately 9 to 11 days after ovulation;
if conception does not occur, the corpus luteum undergoes involution (a
progres-sive decrease in size) and progesterone production sharply declines.
This withdrawal of progesterone releases FSH from negative feedback, thus FSH
levels begin to rise prior to menstruation and the initiation of a new cycle.
The carefully orchestrated
sequence of estrogen pro-duction and then progesterone production is essential
for proper endometrial development to allow implantation of an embryo. If the
oocyte becomes fertilized and implanta-tion occurs, the resulting zygote begins
secreting human chorionic gonadotropin (hCG), which sustains the corpus luteum
for another 6 to 7 weeks. Adequate progesterone production by the corpus luteum
is necessary to sustain the early pregnancy. By 9 to 10 weeks of pregnancy,
placental steroidogenesis is well-established and the placenta assumes
progesterone production.
The corpus luteum measures
approximately 2.5 cm in diameter, has a characteristic deep yellow color, and
can be seen on gross inspection of the ovary if surgery is performed during the
luteal phase of the cycle. As the function of the corpus luteum declines, it
decreases in volume and loses its yellow color. After a few months, the corpus
luteum becomes a white fibrous streak within the ovary, called the corpus albicans.
Reproductive cycle changes in
gonadotropins, steroid hormones, ovarian follicles, and the endometrium are
sum-marized in Figure 33.4.
Related Topics