Chapter: Obstetrics and Gynecology: Reproductive Cycles
Clinical Manifestations of Hormonal Changes
CLINICAL MANIFESTATIONS OF HORMONAL CHANGES
Hormonal changes induced by the hypothalamic-pituitary-ovarian
axis and the adrenal gland trigger puberty, and hormones continue to exert a
cyclic influence until a woman reaches menopause. At that time, the lack of
cyclic ovarian function results in the permanent cessation of menstruation.
Various
female structures undergo changes in response to the reproductive cycle
hormones: the endometrium and endocervix, breasts, vagina, and the
hypothalamus. Changes in the endo-cervix and breasts can be
directly observed. Daily assess-ment of basal body temperature can identify
changes in the hypothalamic thermoregulation center. Other changes can be
assessed by cytologic examination of a sample from the vaginal epithelium or
histologic evaluation of an endome-trial biopsy. A careful history may identify
symptoms asso-ciated with hormone effects, such as abdominal bloating, fluid
retention, mood and appetite changes, and uterine cramps at the onset of
menstruation.
Endometrium
Within the uterus, the
endometrium undergoes dramatic histologic changes during the reproductive
cycle. During menstruation, the entire endometrium is expelled and only the
basal layer remains. During the follicular phase, the rise in estrogen levels
stimulates endometrial cell growth: the endometrial stroma thickens and the endometrial
glands become elongated to form the proliferative endometrium. In an ovulatory
cycle, the endometrium reaches maximal thickness at the time of ovulation.
When ovulation occurs, the
predominant hormone shifts from estrogen to progesterone and distinct changes
occur within the endometrium at almost daily intervals. Progesterone causes
differentiation of the endometrial components and converts the proliferative
endometrium into a secretory endometrium. The endometrial stroma becomes loose
and edematous, while blood vessels enter-ing the endometrium become thickened
and twisted. The endometrial glands, which were straight and tubular dur-ing
the proliferative phase, become tortuous and contain secretory material within
the lumen. With the withdrawal of progesterone at the end of the luteal phase,
the endo-metrium breaks down and is sloughed during menses.
If ovulation does not occur and estrogen continues to be produced, the endometrial stroma continues to thicken and the endometrial glands continue to elongate. Only an endometrial biopsy will identify proliferative endometrium. The endometrium eventually outgrows its blood supply and sections of the endometrium slough intermittently. Without progesterone withdrawal to initiate desquamation of the entire endometrium, bleeding is acyclic and occurs outside of hormonal control irregularly and for prolonged periods of time. When women present with abnormal uterine bleeding, anovulatory bleeding is a common diagnosis.
Endocervix
The endocervix contains glands
that secrete mucus in response to hormonal stimulation. Under the influence of
estrogens, the endocervical glands secrete large quantities of thin, clear,
watery mucus. Endocervical mucus produc-tion is maximal at the time of
ovulation. This mucus facili-tates sperm capture, storage, and transport. With
ovulation, progesterone reverses the effect of estrogen on the endo-cervical
mucus, and mucus production diminishes.
Some women monitor their cervical
mucus to optimize the timing of intercourse when trying to conceive or in order
to avoid conception. However, the timing of these changes is nonspecific and is
an unreliable method of contraception
Breasts
Estrogen exposure is necessary for
pubertal breast devel-opment; however, reproductive cycle changes in the breast
occur primarily due to progesterone effect. The ductal elements of the breast,
nipple, and areola respond to progesterone secretion. Some women will notice
more breast tenderness and fullness in the luteal phase due to
progesterone-mediated changes.
Vagina
Estrogen promotes growth of the
vaginal epithelium and maturation of the superficial epithelial cells of the
mucosa. During sexual stimulation, the presence of estrogen aids vaginal
transudation and lubrication, which facilitates inter-course. During the luteal
phase of the reproductive cycle, the vaginal epithelium retains its thickness,
but the secre-tions are markedly diminished.
Hypothalamic Thermoregulation Center
Progesterone is a hormone with
thermogenic effects; under the influence of progesterone, the hypothalamus
shifts the basal body temperature upward by 0.5°F to 1.0°F over
the average preovulatory temperature. This shift occurs abruptly with the
beginning of progesterone secretion and quickly returns to baseline with the
decline in progesterone secretion. Therefore, these changes in basal body
temper-ature reflect changes in plasma progesterone concentration.
Since the
basal body temperature assumes basal conditions at rest, it should be performed
immediately in the morning upon awakening, prior to any activity.
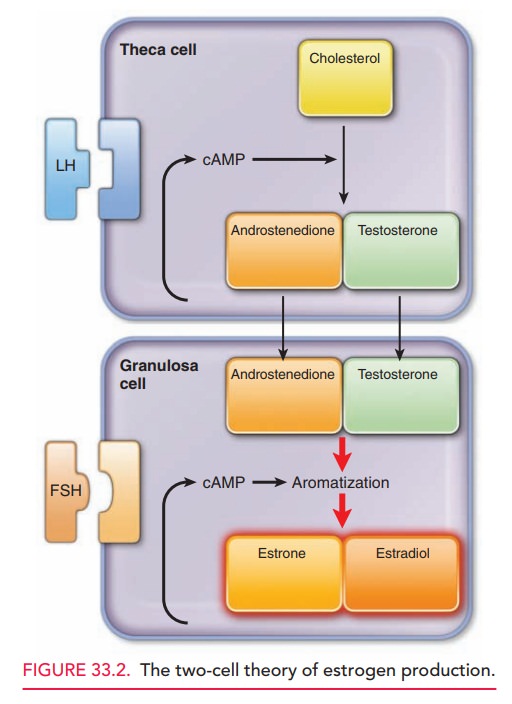
Special thermometers with an
expanded scale are available for this purpose. Identification of this
characteristic bipha-sic curve provides retrospective, indirect evidence of
ovula-tion; however, some ovulatory women do not demonstrate these changes (see
Fig. 33.2)
Related Topics