Chapter: Psychiatric Mental Health Nursing : Foundations of Psychiatric Mental Health Nursing
Psychiatric Nursing Practice
In 1873, Linda Richards graduated from the New England Hospital for
Women and Children in Boston. She went on to improve nursing care in
psychiatric hospitals and orga-nized educational programs in state mental
hospitals in Illi-nois. Richards is called the first American psychiatric
nurse; she believed that “the mentally sick should be at least as well cared
for as the physically sick” (Doona, 1984).
The first training of nurses to work with persons with mental
illness was in 1882 at McLean Hospital in Belmont, Massachusetts. The care was
primarily custodial and focused on nutrition, hygiene, and activity. Nurses
adapted medical– surgical principles to the care of clients with psychiatric
dis-orders and treated them with tolerance and kindness. The role of
psychiatric nurses expanded as somatic therapies for the treatment of mental
disorders were developed. Treat-ments, such as insulin shock therapy (1935),
psychosurgery (1936), and electroconvulsive therapy (1937), required nurses to
use their medical–surgical skills more extensively.
The first psychiatric nursing textbook, Nursing Mental Diseases by
Harriet Bailey, was published in 1920. In 1913, Johns Hopkins was the first school of nursing to include a course
in psychiatric nursing in its curriculum. It was not until 1950 that the
National League for Nursing, which accredits nursing programs, required schools
to include an experience in psychiatric nursing.
Two early nursing theorists shaped psychiatric nursing practice:
Hildegard Peplau and June Mellow. Peplau pub-lished Interpersonal Relations in Nursing in 1952 and Inter-personal Techniques: The Crux of Psychiatric Nursing in 1962. She described the therapeutic
nurse–client relationship with its phases and tasks and wrote extensively about
anxiety . The interpersonal dimension that was crucial to her beliefs forms the
foundations of practice today.
Mellow’s 1968 work, Nursing
Therapy, described her approach of focusing on clients’ psychosocial needs
and strengths. Mellow contended that the nurse as therapist is particularly
suited to working with those with severe mental illness in the context of daily
activities, focusing on the here and now to meet each person’s psychosocial
needs (1986). Both Peplau and Mellow substantially con-tributed to the practice
of psychiatric nursing.
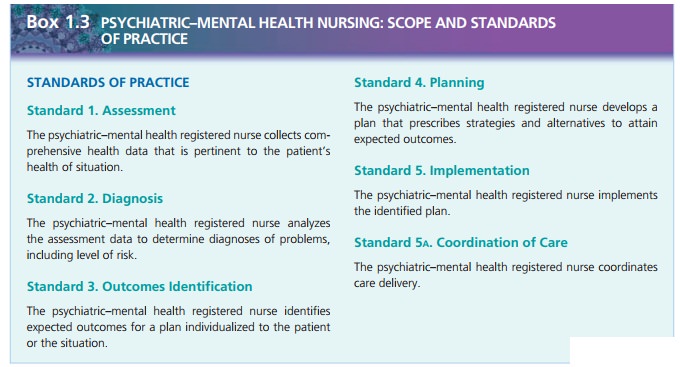
In 1973, the division of psychiatric and mental health practice of
the American Nurses Association (ANA) devel-oped standards of care, which it
revised in 1982, 1994, 2000, and 2007. Standards
of care are authoritative state-ments by professional organizations that
describe the responsibilities for which nurses are accountable. They are not
legally binding unless they are incorporated into the state nurse practice act
or state board rules and regula-tions. When legal problems or lawsuits arise,
these profes-sional standards are used to determine safe and acceptable
practice and to assess the quality of care.
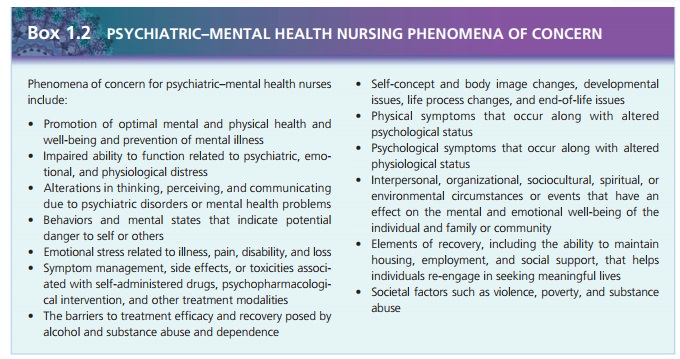
This document also outlines the areas of practice and phenomena of
concern for today’s psychiatric–mental health nurse. The phenomena of concern describe the 13 areas of concern that mental
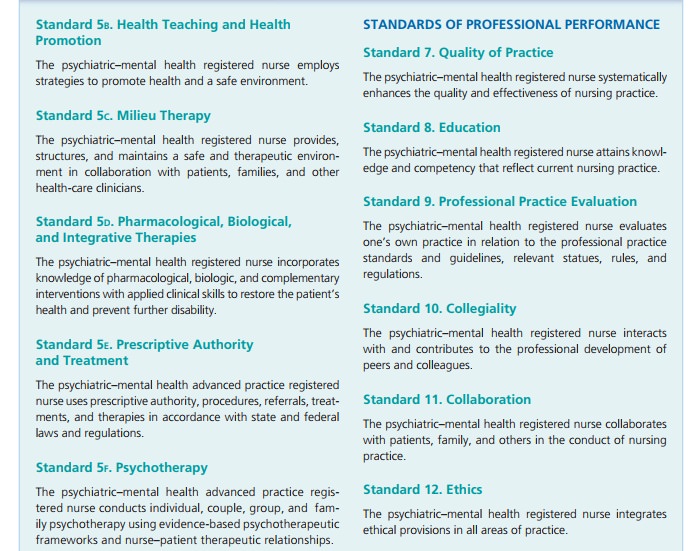
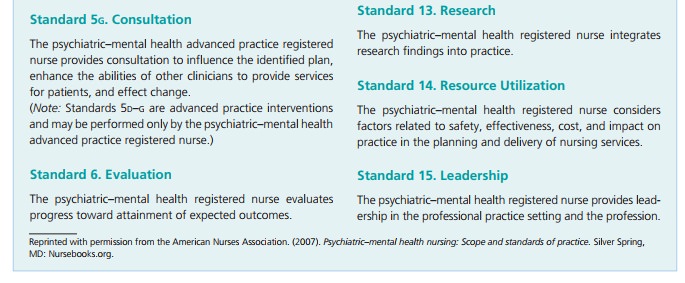
health nurses focus on when caring for clients. The standards of care
incorporate the phases of the nursing process, including specific types of
interventions, for nurses in psychiatric settings and outline standards for
professional performance: quality of care, per-formance appraisal, education,
collegiality, ethics, collabo-ration, research, and resource utilization.
Related Topics