Chapter: Psychiatric Mental Health Nursing : Foundations of Psychiatric Mental Health Nursing
Mental Illness in the 21st Century
MENTAL ILLNESS IN THE 21ST CENTURY
The National Institute of
Mental Health (NIMH, 2008) estimates that more than 26% of Americans aged 18
years and older have a diagnosable mental disorder— approximately 57.7 million
persons each year. Further-more, mental illness or serious emotional
disturbances impair daily activities for an estimated 15 million adults and 4
million children and adolescents. For example, attention deficit hyperactivity
disorder affects 3% to 5% of school-aged children. More than 10 million
children younger than 7 years grow up in homes where at least one parent
suffers from significant mental illness or sub-stance abuse, a situation that
hinders the readiness of these children to start school. The economic burden of
mental illness in the United States, including both health-care costs and lost
productivity, exceeds the economic burden caused by all kinds of cancer. Mental
disorders are the leading cause of disability in the United States and Canada for
persons 15 to 44 years of age. Yet only one in four adults and one in five
children and adolescents requiring mental health services get the care they
need.
Some believe that
deinstitutionalization has had nega-tive as well as positive effects. Although
deinstitutionaliza-tion reduced the number of public hospital beds by 80%, the
number of admissions to those beds correspondingly increased by 90%. Such
findings have led to the term revolving
door effect. Although people with severe and per-sistent mental illness
have shorter hospital stays, they are admitted to hospitals more frequently.
The continuous flow of clients being admitted and discharged quickly overwhelms
general hospital psychiatric units. In some cities, emergency department visits
for acutely disturbed persons have increased by 400 to 500%.
Shorter hospital stays
further complicate frequent, repeated hospital admissions. People with severe
and persis-tent mental illness may show signs of improvement in a few days but
are not stabilized. Thus, they are discharged into the community without being
able to cope with community living. The result frequently is decompensation and
rehospi-talization. In addition, many people have a dual problem of both severe
mental illness and substance abuse. Use of alco-hol and drugs exacerbates
symptoms of mental illness, again making rehospitalization more likely.
Substance abuse issues cannot be dealt with in the 3 to 5 days typical for
admissions in the current managed care environment.
Homelessness is a major
problem in the United States today. One third of adult homeless persons are
estimated to have a serious mental illness and more than one half also have
sub-stance abuse problems. The segment of the homeless popula-tion considered
to be chronically homeless numbers 200,000, and 85% of this group has a
psychiatric illness or a substance abuse problem. Those who are homeless and
mentally ill are found in parks, airport and bus terminals, alleys and
stairwells, jails, and other public places. Some use shelters, halfway houses,
or board-and-care rooms; others rent cheap hotel rooms when they can afford it.
Homelessness worsens psychi-atric problems for many people with mental illness
who end up on the streets, contributing to a vicious cycle. The Treatment
Advocacy Center (2008) reports that rates of mental illness, par-ticularly
major depression, bipolar disorder, and substance abuse, are increasing among
the homeless population.
Many of the problems of the
homeless mentally ill, as well as of those who pass through the revolving door
of psy-chiatric care, stem from the lack of adequate community resources. Money
saved by states when state hospitals were closed has not been transferred to
community programs and support. Inpatient psychiatric treatment still accounts
for most of the spending for mental health in the United States, so community
mental health has never been given the financial base it needs to be effective.
In addition, men-tal health services provided in the community must be
indi-vidualized, available, and culturally relevant to be effective.
In 1993, the federal
government created and funded Access to Community Care and Effective Services
and Support (ACCESS) to begin to address the needs of people with mental
illness who were homeless either all or part of the time. The goals of ACCESS
were to improve access to comprehensive services across a continuum of care,
reduce duplication and cost of services, and improve the efficiency of services.
Programs such as these provide services to people who otherwise would not
receive them and have proved successful in treating psychiatric illness and in
decreasing homelessness.
Objectives for the Future
Unfortunately, only one in
four affected adults and one in five children and adolescents receive treatment
(Depart-ment of Health and Human Services [DHHS], 2008).
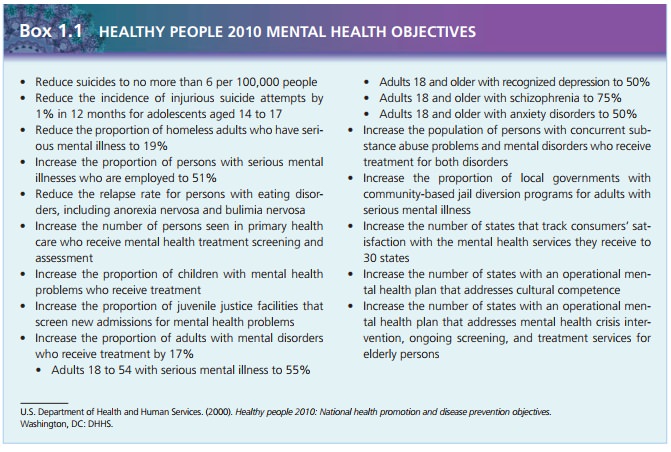
Statistics like these
underlie the Healthy People 2010 objec-tives for mental health proposed by the
U.S. DHHS. These objectives, originally developed as Healthy People 2000, were
revised in January 2000 to increase the number of people who are identified,
diagnosed, treated, and helped to live healthier lives. The objectives also
strive to decrease rates of suicide and homelessness, to increase employment
among those with serious mental illness, and to provide more services both for
juveniles and for adults who are incarcerated and have mental health problems.
At this time, work has begun on Healthy People 2020 goals, which will be
released in January 2010.![]()
![]()
Community-Based Care
After deinstitutionalization,
the 2,000 community mental health centers that were supposed to be built by
1980 had not materialized. By 1990, only 1,300 programs provided various types
of psychosocial rehabilitation services. Per-sons with severe and persistent
mental illness were either ignored or underserved by community mental health
cen-ters. This meant that many people needing services were, and still are, in
the general population with their needs unmet. The Treatment Advocacy Center
(2008) reports that about one half of all persons with severe mental ill-ness
have received no treatment of any kind in the previ-ous 12 months. Persons with
minor or mild cases are more likely to receive treatment, whereas those with severe
and persistent mental illness are least likely to be treated.
Community support service
programs were developed to meet the needs of persons with mental illness
outside the walls of an institution. These programs focus on reha-bilitation,
vocational needs, education, and socialization as well as on management of
symptoms and medication. These services are funded by states (or counties) and
some private agencies. Therefore, the availability and quality of services vary
among different areas of the country. For example, rural areas may have limited
funds to provide mental health services and smaller numbers of people needing
them. Large metropolitan areas, although having larger budgets, also have
thousands of people in need of service; rarely is there enough money to provide
all the services needed by the population.
Unfortunately, the
community-based system did not accu-rately anticipate the extent of the needs
of people with severe and persistent mental illness. Many clients do not have
the skills needed to live independently in the community, and teaching these
skills is often time consuming and labor inten-sive, requiring a 1:1
staff-to-client ratio. In addition, the nature of some mental illnesses makes
learning these skills more difficult. For example, a client who is
hallucinating or “hearing voices” can have difficulty listening to or
compre-hending instructions. Other clients experience drastic shifts in mood,
being unable to get out of bed one day and then unable to concentrate or pay
attention a few days later.
Despite the flaws in the
system, community-based pro-grams have positive aspects that make them
preferable for treating many people with mental illness. Clients can remain in
their communities, maintain contact with family and friends, and enjoy personal
freedom that is not possi-ble in an institution. People in institutions often
lose moti-vation and hope as well as functional daily living skills, such as
shopping and cooking. Therefore, treatment in the community is a trend that
will continue.
Cost Containment and Managed Care
Health-care costs spiraled
upward throughout the 1970s and 1980s in the United States. Managed care is a concept designed to
purposely control the balance between the quality of care provided and the cost
of that care. In a man-aged care system, people receive care based on need
rather than on request. Those who work for the organization pro-viding the care
assess the need for care. Managed care began in the early 1970s in the form of
health maintenance organizations, which were successful in some areas with
healthier populations of people.
In the 1990s, a new form of
managed care, called utilization review
firms or managed care organizations,
was developed to control the expenditure of insurance funds by requiring
providers to seek approval before the delivery of care. Case management, or management ofcare on a case-by-case basis,
represented an effort to pro-vide necessary services while containing cost. The
client is assigned to a case manager, a person who coordinates all types of
care needed by the client. In theory, this approach is designed to decrease
fragmented care from a variety of sources, eliminate unneeded overlap of
services, provide care in the least restrictive environment, and decrease costs
for the insurers. In reality, expenditures are often reduced by withholding
services deemed unnecessary or substituting less expensive treatment
alternatives for more expensive care, such as hospital admission.
Psychiatric care is costly
because of the long-term nature of the disorders. A single hospital stay can
cost $20,000 to $30,000. Also, there are fewer objective measures of health or
illness. For example, when a per-son is suicidal, the clinician must rely on
the person’s report of suicidality; no laboratory tests or other diagnos-tic
studies can identify suicidal ideas. Mental health care is separated from
physical health care in terms of insur-ance coverage: There are often specific
dollar limits or permitted numbers of hospital days in a calendar year. When
private insurance limits are met, public funds through the state are used to
provide care. As states expe-rience economic difficulties, the availability of
state funds for mental health care decreases as well.
Mental health care is managed
through privately owned behavioral health-care firms that often provide the
servicesand manage their cost. Persons without private insurance must rely on
their counties of residence to provide funding through tax dollars. These
services and the money to fund them often lag far behind the need that exists.
In addition, many persons with mental illness do not seek care and in fact
avoid treatment. These persons are often homeless or in jail. Two of the
greatest challenges for the future are to provide effective treatment to all
who need it and to find the resources to pay for this care.
The Health Care Finance
Administration administers two insurance programs: Medicare and Medicaid.
Medicare cov-ers people 65 years and older, people with permanent kidney
failure, and people with certain disabilities. Medicaid is jointly funded by
the federal and state governments and cov-ers low-income individuals and
families. Medicaid varies depending on the state; each state determines
eligibility requirements, scope of services, and rate of payment for ser-vices.
Medicaid covers people receiving either SSI or SSDI until they reach 65 years
of age, although people receiving SSDI are not eligible for 24 months. SSI recipients,
however, are eligible immediately. Unfortunately, not all people who are
disabled apply for disability benefits, and not all people who apply are
approved. Thus, many people with severe and persistent mental illness have no
benefits at all.
Another funding issue is
mental health parity, or equal-ity, in insurance coverage provided for both
physical and mental illnesses. In the past, insurers had spending caps for
mental illness and substance abuse treatment. Some policies placed an annual
dollar limitation for treatment, whereas others limited the number of days that
would be covered annually or in the insured person’s lifetime (of the policy).
In 1996, Congress passed the Mental Health Parity Act, which eliminated annual
and lifetime dollar amounts for mental health care for companies with more than
50 employees. However, substance abuse was not covered by this law, and
companies could still limit the number of days in the hospital or the number of
clinic visits per year. Thus, parity did not really exist. Insurance is
governed by the laws of each state, so some states have full parity, while
others have “limited” parity for mental health coverage— and some states have
no parity laws on the books (National Alliance for the Mentally Ill [NAMI], 2007).
Cultural Considerations
The U.S. Census Bureau (2000)
estimates that 62% of the population has European origins. This number is
expected to continue to decrease as more U.S. residents trace their ancestry to
African, Asian, Arab, or Hispanic origins. Nurses must be prepared to care for
this culturally diverse popula-tion, which includes being aware of cultural
differences that influence mental health and the treatment of mental illness.
Diversity is not limited to culture; the structure of fami-lies has changed as well. With a divorce rate of 50% in the United States, single parents head many families and manyblended families are created when divorced persons remarry. Twenty-five percent of households consist of a single person (U.S. Census Bureau, 2000), and many people live together without being married. Gay men and lesbians form partner-ships and sometimes adopt children. The face of the family in the United States is varied, providing a challenge to nurses to provide sensitive, competent care.
![]()
![]()
Related Topics