Chapter: Medical Surgical Nursing: Preoperative Nursing Management
Preparation for Surgery
Preparation for Surgery
INFORMED CONSENT
Voluntary
and written informed consent from
the patient is necessary before nonemergent surgery can be performed. Such
written consent protects the patient from unsanctioned surgery and protects the
surgeon from claims of an unauthorized oper-ation. In the best interests of all
parties concerned, sound med-ical, ethical, and legal principles are followed.
The nurse may ask the patient to sign the form and may witness the patient’s
signature. It is the physician’s responsibility to provide appro-priate
information. Chart 18-2 lists the criteria for a valid in-formed consent.
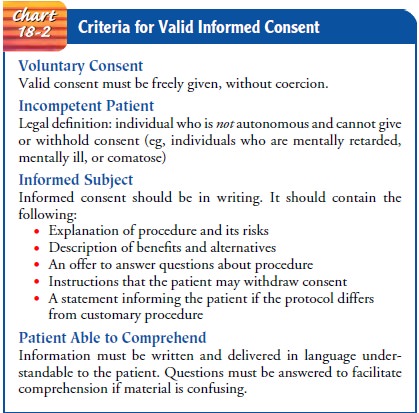
Many ethical principles are integral to informed consent. Before the patient signs the consent form, the surgeon must provide a clear and simple explanation of what the surgery will entail. The surgeon must also inform the patient of the ben-efits, alternatives, possible risks, complications, disfigurement, disability, and removal of body parts as well as what to expect in the early and late postoperative periods. If the patient needs additional information to make his or her decision, the nurse notifies the physician about this. Also, the nurse ascertains that the consent form has been signed before administering psycho-active premedication, because the consent may not be valid if it was obtained while the patient was under the influence of medications that can affect judgment and decision-making capacity. Informed consent is necessary in the following circumstances:
• Invasive procedures, such as a surgical
incision, a biopsy, a cystoscopy, or paracentesis
• Procedures requiring sedation and/or
anesthesia
• A nonsurgical procedure, such as an
arteriography, that car-ries more than slight risk to the patient
• Procedures involving radiation
The patient personally signs the consent if he or she is of legal age and is mentally capable. When the patient is a minor or un-conscious or incompetent, permission must be obtained from a responsible family member (preferably next of kin) or legal guardian. An emancipated minor (married or independently earning his or her own living) may sign his or her own consent form. State regulations and agency policy must be followed.
In an
emergency, it may be necessary for the surgeon to operate as a lifesaving
measure without the patient’s informed consent. Every effort, however, must be
made to contact the patient’s family. In such a situation, contact can be made
by telephone, telegram, fax, or other electronic means.
When
the patient has doubts and has not had the opportunity to investigate
alternative treatments, a second opinion may be re-quested. No patient should
be urged or coerced to sign an oper-ative permit. Refusing to undergo a
surgical procedure is a person’s legal right and privilege. However, such
information must be documented and relayed to the surgeon so that other
arrangements can be made. For example, additional explanations may be provided
to the patient and family, or the surgery may be rescheduled.
The
consent process can be improved by providing audio-visual materials to
supplement discussion, by ensuring that the wording of the consent form is
understandable, and by using other strategies and resources as needed to help
the patient understand its content.
ASSESSMENT OF HEALTH FACTORS THAT AFFECT PATIENTS PREOPERATIVELY
The
overall goal in the preoperative period is for the patient to have as many
positive health factors as possible. Every attempt is made to stabilize those
conditions that otherwise hinder a smooth recovery. When negative factors
dominate, the risks of surgery and postoperative complications increase.
Before
any surgical treatment is initiated, a health history is obtained, a physical
examination is performed during which vital signs are noted, and a database is
established for future compar-isons (Meeker & Rothrock, 1999). During the
physical exami-nation, many factors are considered that have the potential to
affect the patient undergoing surgery. Health care providers should be alert
for signs of abuse that can occur at all ages and to men and women from all
socioeconomic, ethnic, and cultural groups (Little, 2000; Marshall, Benton
& Brazier, 2000). Findings need to be reported accordingly.
Blood
tests, x-rays, and other diagnostic tests are prescribed when specifically
indicated by information obtained from a thor-ough history and physical
examination (King, 2000). These pre-liminary contacts with the health care team
provide the patient with opportunities to ask questions and to become
acquainted with those who may be providing care during and after surgery.
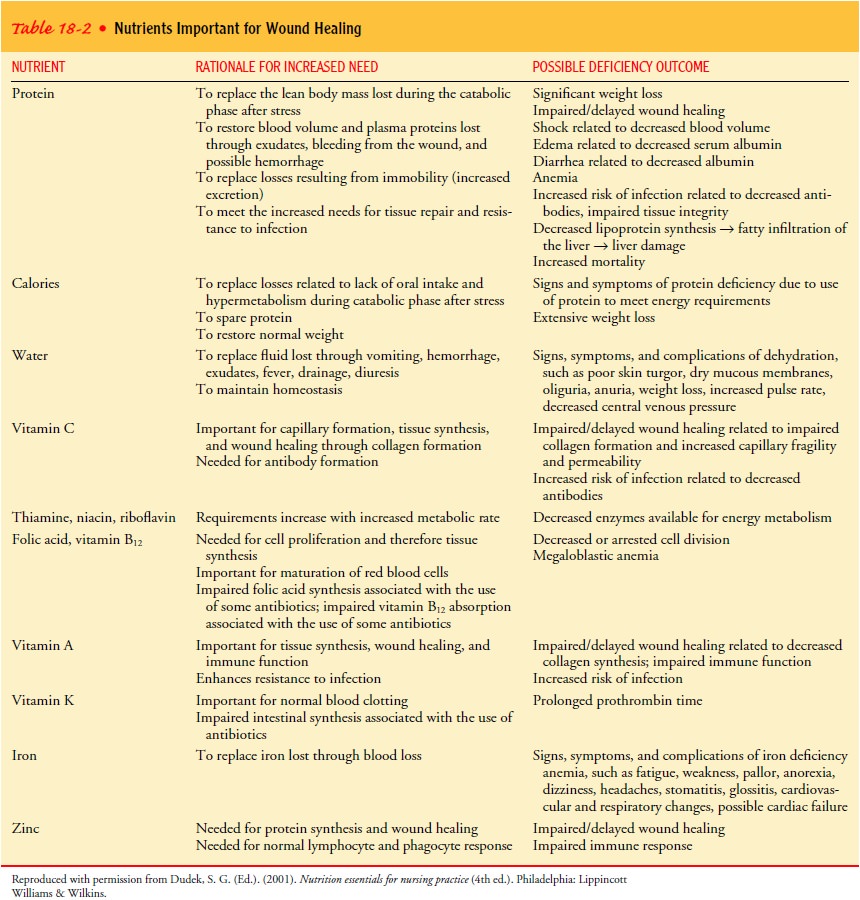
Nutritional and Fluid Status
Optimal
nutrition is an essential factor in promoting healing and resisting infection
and other surgical complications (Braunschweig, Gomez & Sheean, 2000).
Assessment of a patient’s nutritional sta-tus provides information on obesity,
undernutrition, weight loss, malnutrition, deficiencies in specific nutrients,
metabolic abnor-malities, the effects of medications on nutrition, and special
prob-lems of the hospitalized patient (Quinn, 1999). Nutritional needs may be
determined by measurement of body mass index and waist circumference (National
Institutes of Health, 2000).
Any
nutritional deficiency, such as malnutrition, should be corrected before
surgery so that enough protein is available for tissue repair (King, 2000;
Russell, Williams & Bulstrode, 2000). The nutrients needed for wound
healing are summarized in Table 18-2.
Dehydration,
hypovolemia, and electrolyte imbalances can lead to significant problems in
patients with comorbid medical conditions or in elderly patients. The severity
of fluid and electro-lyte imbalances is often difficult to determine. Mild
volume de-ficits may be treated during surgery; however, additional time may be
needed to correct pronounced fluid and electrolyte deficits to promote the best
possible preoperative condition.
Drug or Alcohol Use
People
who abuse drugs or alcohol frequently deny or attempt to hide it. In such
situations, the nurse who is obtaining the patient’s health history needs to
ask frank questions with patience, care, and a nonjudgmental attitude.
Because
acutely intoxicated persons are susceptible to injury, surgery is postponed in
these patients if possible. If emergency surgery is required, local, spinal, or
regional block anesthesia is used for minor surgery. Otherwise, to prevent
vomiting and po-tential aspiration, a nasogastric tube is inserted before
adminis-tering general anesthesia.
The
person with a history of chronic alcoholism often suffers from malnutrition and
other systemic problems that increase the surgical risk. Additionally, alcohol
withdrawal delirium (delirium tremens) may be anticipated up to 72 hours after
alcohol with-drawal. Delirium tremens is associated with a significant
mortal-ity rate when it occurs postoperatively.
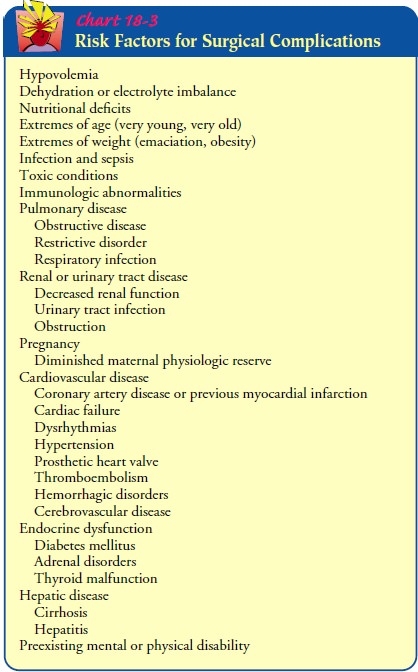
Chart
18-3 gives more information about risk factors that may lead to complications.
Respiratory Status
The
goal for potential surgical patients is optimal respiratory function. Patients
are taught breathing exercises and use of an incentive spirometer if indicated.
Because adequate ventilation is potentially compromised during all phases of
surgical treat-ment, surgery is usually postponed when the patient has a
respi-ratory infection. Patients with underlying respiratory disease (eg,
asthma, chronic obstructive pulmonary disease) are assessed carefully for
current threats to their pulmonary status. Patients’ use of medications that
may affect recovery is also assessed (King, 2000; Smetana, 1999).
Patients
who smoke are urged to stop 2 months before sur-gery (King, 2000), although
many do not do so. These patients should be counseled to stop smoking at least
24 hours prior to surgery. Research suggests that counseling has a positive
effect on the patient’s smoking behavior 24 hours preceding surgery, helping
reduce the potential for adverse effects associated with smoking such as
increased airway reactivity, decreased muco-ciliary clearance, as well as
physiologic changes in the cardio-vascular and immune systems (Shannon-Cain,
Webster & Cain, 2002).
Cardiovascular Status
The goal in preparing any patient for surgery is to ensure a well-functioning cardiovascular system to meet the oxygen, fluid, and nutritional needs of the perioperative period. If the patient has uncontrolled hypertension, surgery may be postponed until the blood pressure is under control.
Because
cardiovascular disease increases the risk for complica-tions, patients with
these conditions require greater-than-usual diligence during all phases of
nursing management and care (King, 2000). Depending on the severity of the
symptoms, surgery may be deferred until medical treatment can be instituted to
improve the patient’s condition. At times, surgical treatment can be mod-ified
to meet the cardiac tolerance of the patient. For example, in a patient with
obstruction of the descending colon and coronary artery disease, a temporary
simple colostomy may be performed rather than a more extensive colon resection
that would require a prolonged period of anesthesia.
Hepatic and Renal Function
The
presurgical goal is optimal function of the liver and urinary systems so that
medications, anesthetic agents, body wastes, and toxins are adequately
processed and removed from the body.
The
liver is important in the biotransformation of anesthetic compounds. Therefore,
any disorder of the liver has an effect on how anesthetic agents are
metabolized. Because acute liver disease is associated with high surgical
mortality, preoperative improve-ment in liver function is a goal. Careful
assessment is made with the help of various liver function tests.
Because the kidneys are involved in excreting anesthetic drugs and their metabolites and because acid–base status and metabolism are also important considerations in anesthesia administration, surgery is contraindicated when a patient has acute nephritis, acute renal insufficiency with oliguria or anuria, or other acute renal problems. The exception is surgery that is performed as a lifesav-ing measure or that is necessary to improve urinary function, as in the case of an obstructive uropathy.
Endocrine Function
The
patient with diabetes who is undergoing surgery is at risk for hypoglycemia and
hyperglycemia. Hypoglycemia may develop during anesthesia or postoperatively
from inadequate carbohy-drates or from excessive administration of insulin.
Hyperglycemia, which may increase the risk for surgical wound infection, may
re-sult from the stress of surgery, which may trigger increased levels of
catecholamine. Other risks are acidosis and glucosuria. Although the surgical
risk in the patient with controlled diabetes is no greater than in the
nondiabetic patient, the goal is to maintain the blood glucose level at less
than 200 mg/dL. Frequent monitoring of blood glucose levels is important
before, during, and after surgery.
Patients
who have received corticosteroids are at risk for adre-nal insufficiency.
Therefore, the use of corticosteroids for any purpose during the preceding year
must be reported to the anes-thesiologist or anesthetist and surgeon.
Additionally, the patient is monitored for signs of adrenal insufficiency.
Patients
with uncontrolled thyroid disorders are at risk for thy-rotoxicosis (with hyperthyroid
disorders) and respiratory failure (with hypothyroid disorders). Therefore, the
patient is assessed for a history of these disorders.
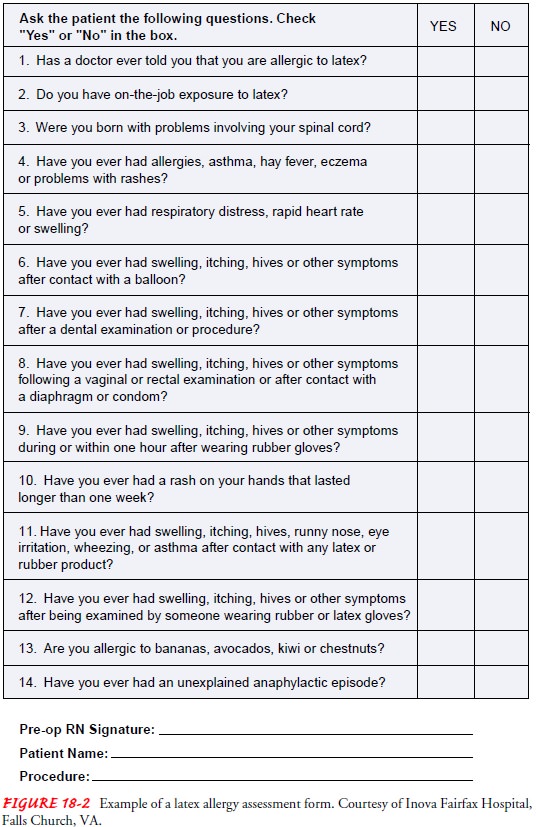
Immune Function
An
important function of the preoperative assessment is to de-termine the
existence of allergies, including the nature of previous allergic reactions. It
is especially important to identify and docu-ment any sensitivity to
medications and past adverse reactions to these agents. The patient is asked to
identify any substances that precipitated previous allergic reactions,
including medications, blood transfusions, contrast agents, latex, and food
products, and to describe the signs and symptoms produced by these substan-ces.
A sample latex allergy screening questionnaire is shown in Figure 18-2.
Immunosuppression
is common with corticosteroid therapy, renal transplantation, radiation
therapy, chemotherapy, and dis-orders affecting the immune system, such as
acquired immuno-deficiency syndrome (AIDS) and leukemia. The mildest symptoms
or slightest temperature elevation must be investigated. Because pa-tients who
are immunosuppressed are highly susceptible to infec-tion, great care is taken
to ensure strict asepsis.
Previous Medication Use
A
medication history is obtained from each patient because of the possible
effects of medications on the patient’s perioperative and perianesthesia course
and the possibility of drug interactions (Quinn, 1999). Any medication the
patient is using or has used in the past is documented, including
over-the-counter (OTC) preparations and herbal agents and the frequency with
which they are used. Potent medications have an effect on physiologic
functions; interactions of such medications with anesthetic agents can cause
serious problems, such as arterial hypotension and cir-culatory collapse.
The
potential effects of prior medication therapy are evaluated by the
anesthesiologist or anesthetist, who considers the length of time the patient
has used the medications, the physical condition of the patient, and the nature
of the proposed surgery. Medica-tions that cause particular concern are listed
in Table 18-3.
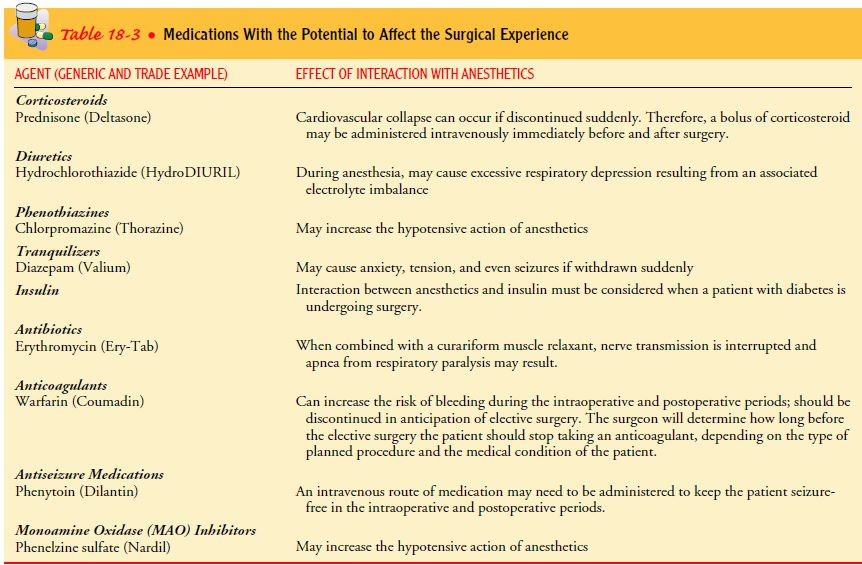
Many
patients take self-prescribed or OTC medications in ad-dition to those listed
in Table 18-3. Aspirin is a common OTC medication prescribed by physicians or
taken independently by patients to prevent myocardial infarction, stroke, and
other dis-orders (Karch, 2002). Because of the effects of aspirin or other OTC
medications and possible interactions with other medica-tions and anesthetic
agents, it is important to ask a patient about their use. The information is
noted in the patient’s chart and con-veyed to the anesthesiologist or
anesthetist and surgeon.
The use of herbal medications is widespread among patients. Approximately 15 million Americans report their use (Ang-Lee, Moss & Yuan, 2001; Karch, 2002; Lyons, 2002). Patients with chronic illnesses may be using herbal medications to supplement their prescribed medications or in place of them.
Certain herbal medications, such as echinacea, ephedra, garlic (Allium sativum), ginkgo, ginseng, kava kava (Piper methysticum), St. John’s wort (Hypericum perforatum), licorice (Glycyhiza glabra), and valerian (Valeriana officinalis) have been
identified as the most commonly used herbal medications that may cause concern
during the peri-operative period (Ang-Lee, Moss & Yuan, 2001; Kuhn, 1999;
Lyons, 2002). Because of the potential effects of herbal medica-tions on
coagulation and potential interactions with other med-ications, the nurse must
ask surgical patients explicitly about the use of these agents, document their
use, and inform the surgical team and anesthesiologist or anesthetist (Brumly,
2000).
Psychosocial Factors
All
patients have some type of emotional reaction before any sur-gical procedure,
be it obvious or hidden, normal or abnormal. For example, preoperative anxiety
may be an anticipatory response to an experience the patient views as a threat
to his or her custom-ary role in life, body integrity, or life itself. Psychological
distress directly influences body functioning. Therefore, it is imperative to
identify any anxiety the patient is experiencing.
By taking a careful health history, the nurse elicits patient con-cerns that can have a bearing on the course of the surgical expe-rience (Quinn, 1999). Undoubtedly, a patient about to undergo surgery is faced with various fears, including fears of the unknown, of death, of anesthesia, pain, or cancer.
Concerns about loss of work time, loss of job, increased responsibilities or burden on family members, and the threat of permanent incapacity further contribute
to the emotional strain created by the prospect of surgery. Less obvious
concerns may occur because of previous ex-periences with the health care system
and people the patient has known with the same condition.
People
express fear in different ways. For example, one patient may repeatedly ask a
lot of questions, even though answers were given previously. Another person may
withdraw, deliberately avoiding communication, perhaps by reading or watching
televi-sion. Still others may talk about trivialities. Consequently, the nurse
must be empathetic, listen well, and provide information that helps alleviate
concerns.
An
important outcome of the psychosocial assessment is the determination of the
extent and role of the patient’s support net-work. The value and reliability of
all available support systems are assessed. Other information, such as usual
level of functioning and typical daily activities, may assist in the patient’s
care and re-habilitation plans. Assessing the patient’s readiness to learn and
determining the best approach to maximize comprehension will provide the basis
for preoperative patient education.
Spiritual and Cultural Beliefs
Spiritual
beliefs play an important role in how people cope with fear and anxiety.
Regardless of the patient’s religious affiliation, spiritual beliefs can be as
therapeutic as medication. Every at-tempt must be made to help the patient obtain
the spiritual help that he or she requests. Faith has great sustaining power.
Thus, the beliefs of each patient should be respected and supported. Somenurses
avoid the subject of a clergy visit lest the suggestion alarm the patient.
Asking if the patient’s spiritual advisor knows about the impending surgery is
a caring, nonthreatening approach.
Showing
respect for a patient’s cultural values and beliefs fa-cilitates rapport and
trust. Some areas of assessment include iden-tifying the ethnic group to which
the patient relates and the customs and beliefs the patient holds about illness
and health care providers. For example, patients from some cultural groups are
unaccustomed to expressing feelings openly. Nurses need to consider this
pattern of communication when assessing pain. As a sign of respect, people from
other cultural groups may not make direct eye contact with others. The nurse
needs to know that this lack of eye contact is not avoidance or a lack of
interest.
Perhaps
the most valuable skill at the nurse’s disposal is listen-ing carefully to the
patient, especially when obtaining the history. Invaluable information and
insights may be gained by engaging in conversation and using communication and
interviewing skills. An unhurried, understanding, and caring nurse invites
confidence on the part of the patient.
Related Topics