Chapter: Medical Surgical Nursing: Preoperative Nursing Management
Immediate Preoperative Nursing Interventions
IMMEDIATE PREOPERATIVE NURSING INTERVENTIONS
The
patient changes into a hospital gown that is left untied and open in the back.
The patient with long hair may braid it, remove hair-pins, and cover the head
completely with a disposable paper cap.
The
mouth is inspected, and dentures or plates are removed. If left in the mouth,
these items could easily fall to the back of the throat during induction of
anesthesia and cause respiratory obstruction.
Jewelry
is not worn to the operating room; wedding rings and jewelry of body piercings
should be removed to prevent injury (Fogg, 2001). If a patient objects to
removing a ring, some insti-tutions allow the ring to be securely fastened to
the finger with tape. All articles of value, including assistive devices,
dentures, glasses, and prosthetic devices, are given to family members or are
labeled clearly with the patient’s name and stored in a safe place according to
the institution’s policy.
All
patients (except those with urologic disorders) should void immediately before
going to the operating room to promote con-tinence during low abdominal surgery
and to make abdominal organs more accessible. Urinary catheterization is
performed in the operating room as necessary.
Administering Preanesthetic Medication
The
use of preanesthetic medication is minimal with ambulatory or outpatient surgery.
If prescribed, it is usually administered in the preoperative holding area. If
a preanesthetic medication is administered, the patient is kept in bed with the
side rails raised because the medication can cause lightheadedness or
drowsiness. During this time, the nurse observes the patient for any untoward
reaction to the medications. The immediate surroundings are kept quiet to
promote relaxation.
Often,
surgery is delayed or operating room schedules are changed, and it becomes
impossible to request that a medica-tion be given at a specific time. In these
situations, the pre-operative medication is prescribed “on call from operating
room.” The nurse can have the medication ready to give and adminis-ter it as
soon as a call is received from the operating room staff. It usually takes 15
to 20 minutes to prepare the patient for the operating room. If the nurse gives
the medication before at-tending to the other details of preoperative
preparation, the pa-tient will have at least partial benefit from the preoperative
medication and will have a smoother anesthetic and operative course.
Maintaining the Preoperative Record
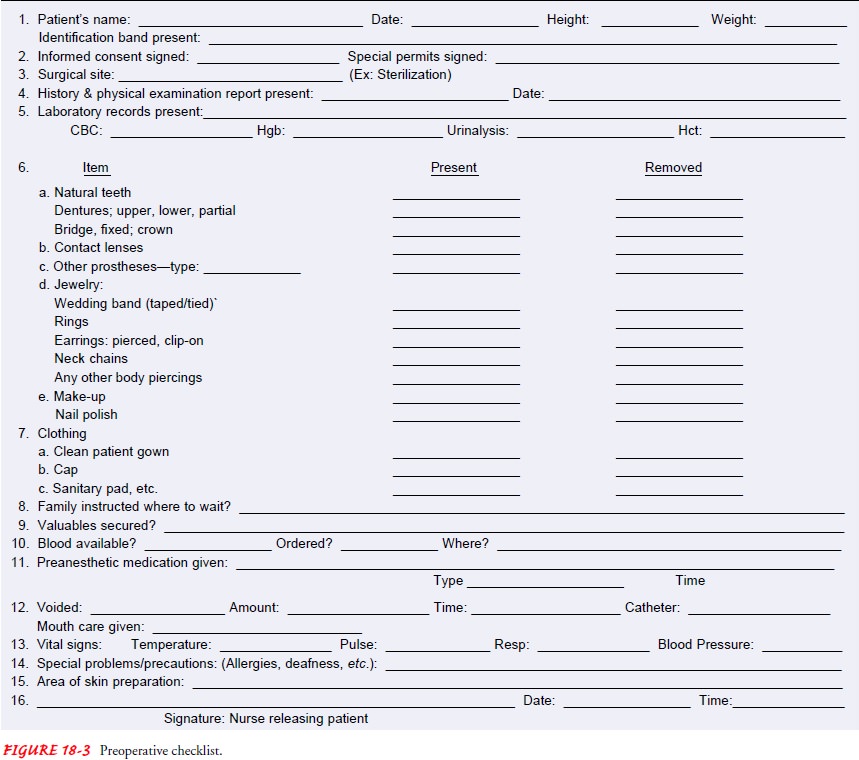
A
preoperative checklist contains critical elements that need to be checked
preoperatively (Meeker & Rothrock, 1999). An example is shown in Figure
18-3. The completed chart accompanies the pa-tient to the operating room with
the surgical consent form attached, along with all laboratory reports and
nurses’ records. Any unusual last-minute observations that may have a bearing
on anesthesia or surgery are noted at the front of the chart in a prominent
place.
Transporting the Patient to the Presurgical Area
The patient is transferred to the holding area or presurgical suite in a bed or on a stretcher about 30 to 60 minutes before the anesthetic is to be given. The stretcher should be as comfortable as possible, with a sufficient number of blankets to prevent chilling in air-conditioned rooms. A small head pillow is usu-ally provided.
The
patient is taken to the preoperative holding area, greeted by name, and
positioned comfortably on the stretcher or bed. The surrounding area should be
kept quiet if the preoperative medication is to have maximal effect. Unpleasant
sounds or con-versation should be avoided because a sedated patient who
over-hears them might misinterpret them.
Patient
safety in the preoperative area is a priority. Using a process to verify
patient identification, the surgical procedure, and the surgical site maximizes
patient safety and allows for early identification and intervention if any
discrepancies are identified (Brown, Riippa & Shaneberger, 2001).
Attending to Family Needs
Most
hospitals and ambulatory surgery centers have a waiting room where the family
and significant others can wait while the patient is undergoing surgery. This
room may be equipped with comfortable chairs, television, telephones, and
facilities for light refreshment. Volunteers may remain with the family, offer
them coffee, and keep them informed of the patient’s progress. After surgery,
the surgeon may meet the family in the waiting room and discuss the outcome.
The
family and significant others should never judge the seri-ousness of an
operation by the length of time the patient is in the operating room. A patient
may be in surgery much longer than the actual operating time for several
reasons:
·
Patients are routinely transported
well in advance of the ac-tual operating time.
·
The anesthesiologist or anesthetist
often makes additional preparations that may take 30 to 60 minutes.
·
The surgeon may take longer than
expected with the preced-ing case, which delays the start of the next surgical
procedure.
After
surgery, the patient is taken to the PACU to ensure safe emergence from
anesthesia.
Family
members and significant others waiting to see the pa-tient after surgery should
be informed that the patient may have certain equipment or devices (eg,
intravenous lines, indwelling urinary catheter, nasogastric tube, oxygen lines,
monitoring equip-ment, and blood transfusion lines) in place when he or she
returns from surgery. When the patient returns to the room, the nurse provides
explanations regarding the frequent postoperative ob-servations that will be
made. However, it is the responsibility of the surgeon, not the nurse, to relay
the surgical findings and the prognosis, even when the findings are favorable.
Related Topics