Chapter: Obstetrics and Gynecology: Postpartum Hemorrhage
Postpartum Hemorrhage: Recognition and Early Detection
RECOGNITION AND EARLY DETECTION
PPH is
not a diagnosis, but a critically important sign that often occurs without
warning and in the absence of risk factors.
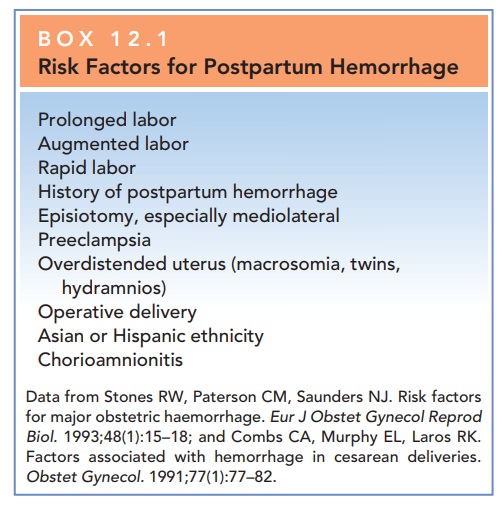
When present, however, these
factors warrant heightened awareness about the risk of PPH (Box 12.1). Maternal
hemodynamic responses to blood loss should also be mon-itored, as these
responses are indicators of well-being, vol-ume deficit, and prognosis. The
loss of 10% to 15% (500 mL for an average patient with singleton pregnancy) of
blood volume may be tolerated with no signs or symp-toms. As blood loss
approaches 20%, the first signs of intravascular depletion become manifest,
including tachy-cardia, tachypnea, and delayed capillary refill, followedby orthostatic changes and narrowed pulse pressure (due to
elevated diastolic pressure secondary to vasoconstric-tion with maintenance of
systolic pressure). Beyond approx-imately 30% volume loss, breathing and heart
rate further increase, and overt hypotension develops. Finally, with profound
blood loss above 40% to 50%, oliguria, shock, coma, and death may occur.
The
source and etiology of bleeding should be identified as soon as possible, and
targeted interventions applied in order to minimize morbidity and prevent
mortality. The most commoncause of PPH is uterine atony,
representing about 80% of cases. Retained placenta, genital tract trauma
(lacera-tions, rupture), and coagulation disorders are other causes. Hematomas
can occur anywhere in the lower genital tract. Ruptured uterus and inverted
uterus are rare but serious causes of PPH.
Related Topics