Chapter: Obstetrics and Gynecology: Postpartum Hemorrhage
General Management of Patients With Postpartum Hemorrhage
GENERAL MANAGEMENT OF PATIENTS WITH POSTPARTUM HEMORRHAGE
Postpartum
hemorrhage is an unequivocal emergency; all available resources should be
mobilized immediately upon its recognition.
A general approach to management is outlined in Box 12.2. Because most cases of PPH are caused by uterine atony, the uterus should be palpated abdominally, seeking the soft, “boggy” consistency of the relaxed uterus. If this find-ing is confirmed, oxytocin infusion should be increased and either methylergonovine maleate or prostaglandins administered if excessive bleeding continues.
Other questions that may help
direct assessment include:
·
Was expulsion of the placenta
spontaneous and appar-ently complete?
·
Were forceps or other
instrumentation used in delivery?
·
Was the baby large or the
delivery difficult or precipitous?
·
Were the cervix and vagina
inspected for lacerations?
·
Is the blood clotting?
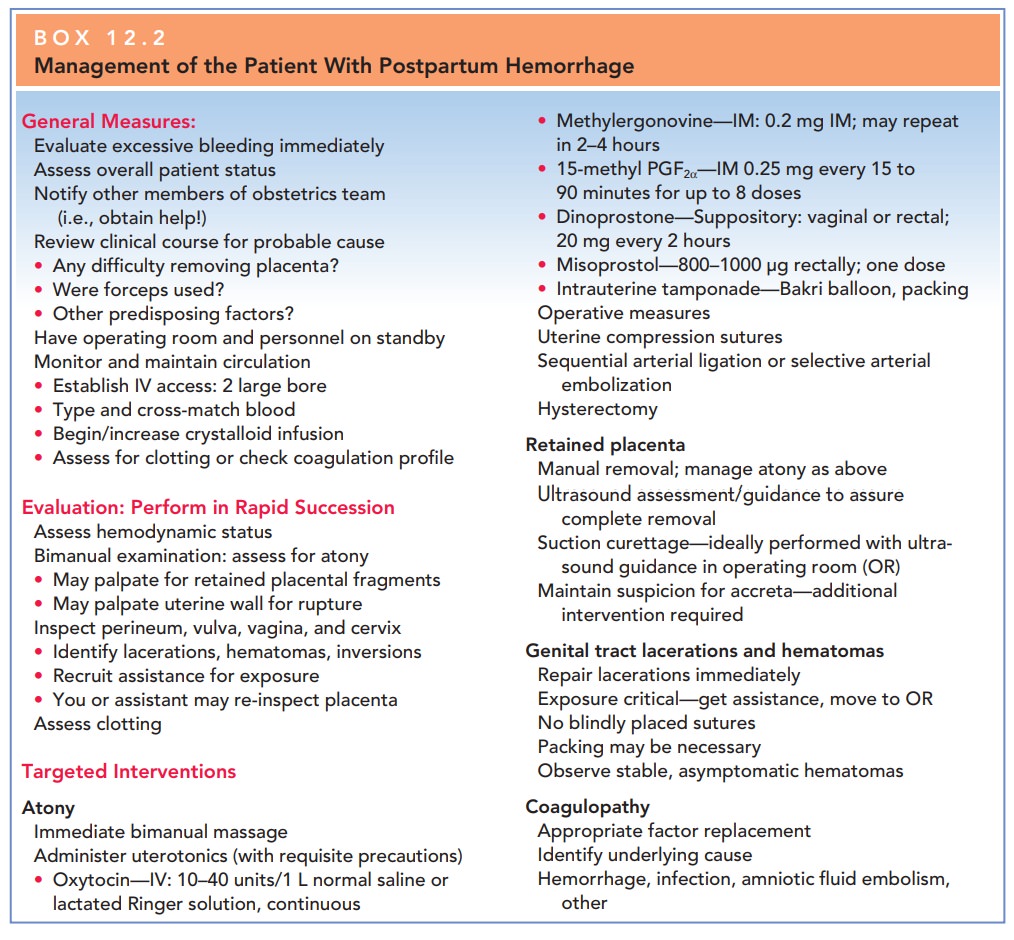
While the cause of the hemorrhage
is being identified, gen-eral supportive measures should be initiated (see Box
12.2). Such measures include large-bore intravenous access; rapid crystalloid
infusions; type, cross match, and admin-istration of blood or blood components
as needed; peri-odic assessment of hematocrit and coagulation profile; and
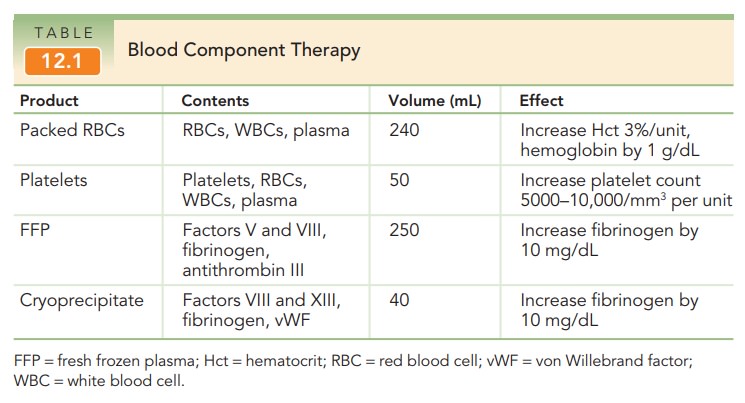
monitoring of urinary output. The judicious use of blood component therapy is
key to management. The mainstay of blood replacement therapy is packed red
blood cells, with other components used as indicated for various dis-orders of
the clotting cascade. See Table 12.1 for an out-line of blood products and
their effects.
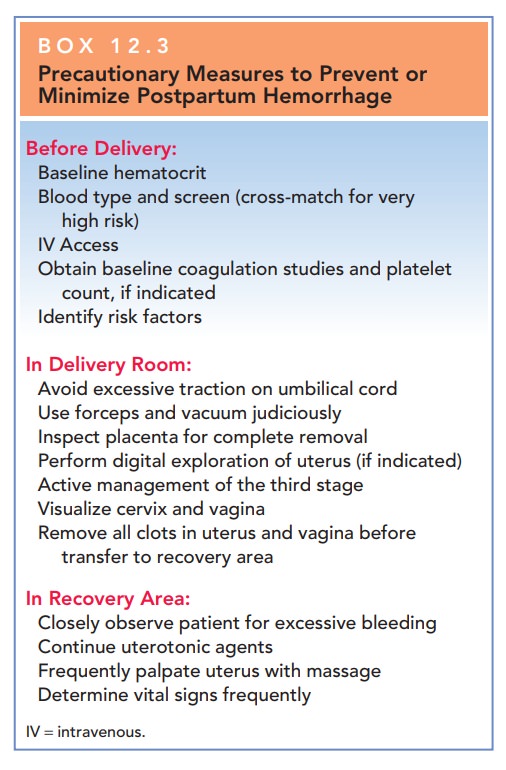
The
management of PPH is greatly facilitated if patients at high risk are
identified and preliminary preparations are made before the bleeding episode. Box 12.3
reviews such pre-liminary, precautionary measures.
Related Topics