Chapter: Medical Microbiology: An Introduction to Infectious Diseases: Pneumocystis carinii
Pneumocystosis : Clinical Aspects
PNEUMOCYSTOSIS : CLINICAL ASPECTS
MANIFESTATIONS
In the immunocompromised host, the disease presents as a progressive, diffuse pneu-monitis. Illness may begin after discontinuation or a decrease in the dose of cortico-steroids or, in the case of acute lymphatic leukemia, during a period of remission. In infants and AIDS patients, onset is typically insidious, and the clinical course is 3 to 4 weeks in duration. Fever is mild or absent. In older individuals and patients who have previously been on high doses of corticosteroids, the onset is more abrupt, and the course is both febrile (38–40°C) and abbreviated. In both populations, the cardinal manifesta-tions are progressive dyspnea and tachypnea; cyanosis and hypoxia eventually supervene.
A nonproductive cough is present in 50% of all patients. Clinical signs of pneumonia are usually absent, despite the presence of infiltrates on x-ray. These infiltrates are alveolar incharacter and spread out symmetrically from the hili, eventually affecting most of the lung. Occasionally, unilateral infiltrates, coin lesions, lobar infiltrates, cavitary lesions, or spontaneous pneumothoraces are observed. Pleural effusions are uncommon. Clinical and radiographic abnormalities are generally accompanied by a decrease in arterial oxygen saturation, diffusion capacity of the lung, and vital capacity. Death occurs by progressive asphyxia.
Lesions outside the lung were rarely seen prior to the AIDS epidemic but are now seen with some regularity. The sites most often involved are lymph nodes, bone marrow, spleen, liver, eyes, thyroid, adrenal glands, gastrointestinal tract, and kidneys. The extra-pulmonary clinical manifestations range from incidental autopsy findings to progressive multisystem disease.
DIAGNOSIS
Definite diagnosis depends on finding organisms of typical morphology in appropriate specimens. Because the pathologic process is alveolar rather than bronchial, the organ-isms are not readily seen in expectorated specimens such as sputum. The diagnostic yield is much better from specimens obtained by more invasive procedures. Of these, bron-choalveolar lavage (BAL) gives the best results with the least morbidity. Percutaneous needle aspiration of the lung, transbronchial biopsy, and open lung biopsy, although somewhat more sensitive techniques, are accompanied by more complications, including pneumothorax and hemothorax.
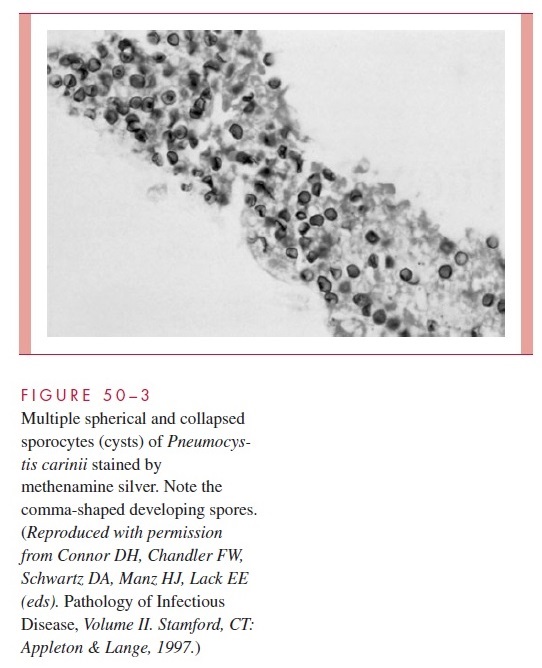
P. carinii can be demonstrated by a wide variety of staining procedures. The standardstain is methenamine silver (Fig 50–3), but a direct fluorescent antibody (DFA) method, if available, is slightly more sensitive. Laboratories often perform a rapid stain (Wright, Giemsa, Papanicolaou) first and confirm by methenamine silver or DFA later. Methods developed for detection of Pneumocystis DNA in BAL and other specimens by poly-merase chain reaction may soon be practical for clinical laboratories.
TREATMENT AND PREVENTION
The fixed combination of trimethoprim and sulfamethoxazole (TMP-SMX) is the treat-ment of choice for all forms of pneumocystosis. It is administered orally or intravenously for 14 to 21 days. Patients with AIDS receive the longer course because they start with a higher organism burden, respond more slowly, and suffer relapse more often. Unfortu-nately, AIDS patients have a high incidence of adverse effects to TMP-SMX, particularly the sulfonamide component. This requires the use of other antimicrobics (eg, clin-damycin, primaquine, dapsone) alone or in combination with TMP. In hospitalized pa-tients, two parenteral drugs, pentamidine and trimetrexate, are the major alternatives to TMP-SMX.
Low-dose administration of TMP-SMX has been shown to significantly decrease the incidence of P. carinii pneumonia in high-risk patients and prevents relapse in AIDS pa-tients. This chemoprophylaxis is indicated for patients who have CD4+ lymphocyte counts below 200/mm3, unexplained fever, or a previous episode of PCP. Once begun, chemoprophylaxis is continued for life.
Related Topics