Chapter: Clinical Dermatology: Other papulosquamous disorders
Pityriasis rubra pilaris
Pityriasis
rubra pilaris
Cause
Several
types have been described, but their causes are unknown. A defect in vitamin A
metabolism was once suggested but has been disproved. The familial type has an
autosomal dominant inheritance.
Presentation
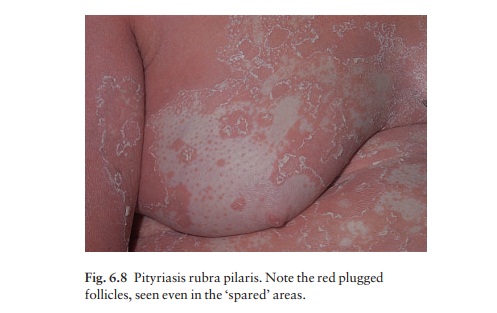
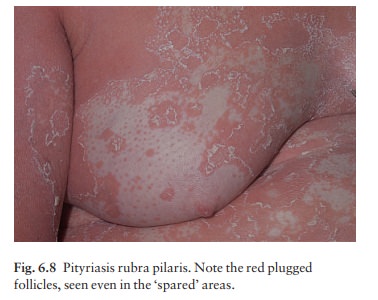
The
familial type develops gradually in childhood and persists throughout life. The
more common acquired type begins in adult life with redness and scaling of the
face and scalp. Later, red or pink areas grow quickly and merge, so that
patients with pityriasis rubra pilaris are often erythrodermic. Small islands
of skin may be ‘spared’ from this general erythema, but even here the follicles
may be red and plugged with keratin (Fig. 6.8). Similarly, the generalized
plaques, although otherwise rather like psoriasis, may also show follicular
plugging.
Course
The
palms and soles become thick, smooth and yellow. They often fissure rather than
bend. The acquired form of pityriasis rubra pilaris generally lasts for 6– 18
months, but may recur. Even when the plaques have gone, the skin may retain a
rough scaly texture with persistent small scattered follicular plugs.
Complications
There are usually no complications. However, wide-spread erythroderma causes the patients to tolerate cold poorly.
Differential diagnosis
Psoriasis
is the disorder closest in appearance to pity-riasis rubra pilaris, but lacks
its slightly orange tinge. The thickening of the palms and soles, the
follicular erythema in islands of uninvolved skin, and follicular plugging
within the plaques, especially over the knuck-les, are other features that help
to separate them.
Investigations
A
biopsy may help to distinguish psoriasis from pityriasis rubra pilaris; but,
even so, the two disorders share many histological features.
Treatment
The
disorder responds slowly to systemic retinoids such as acitretin (in adults,
25–50 mg/day for 6– 8 months;). Oral methotrexate in low doses, once a week may
also help. Topical steroids and kerato-lytics (e.g. 2% salicylic acid in soft
white paraffin) reduce inflammation and scaling, but usually do not suppress
the disorder completely. Systemic steroids are not indicated.
Related Topics