Chapter: Clinical Dermatology: Other papulosquamous disorders
Lichen planus
Lichen
planus
Cause
The
precise cause of lichen planus is unknown, but the disease seems to be mediated
immunologically. Lymphocytes abut the epidermal basal cells and damage them.
Chronic graft-vs.-host disease can cause an eruption rather like lichen planus
in which histoincompatibility causes lymphocytes to attack the epidermis.
Lichen planus is also associated with auto-immune disorders, such as alopecia
areata, vitiligo and ulcerative colitis, more commonly than would be expected
by chance. Drugs too can cause lichen planus . Some patients with lichen planus
also have a hepatitis B or C infectionabut lichen planus itself is not
infectious.
Presentation
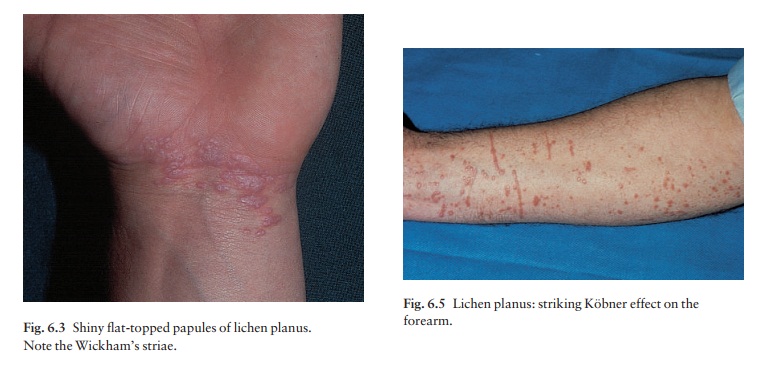
Typical
lesions are violaceous or lilac-coloured, intensely itchy, flat-topped papules
that usually arise on the extremities, particularly on the volar aspects
A close look is needed to see a white streaky
pattern on the surface of these papules (Wickham’s striae). White asymptomatic
lacy lines, dots, and occasionally small white plaques, are also found in the
mouth, particularly inside the
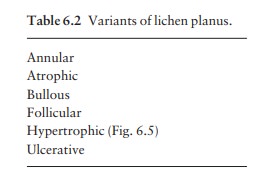
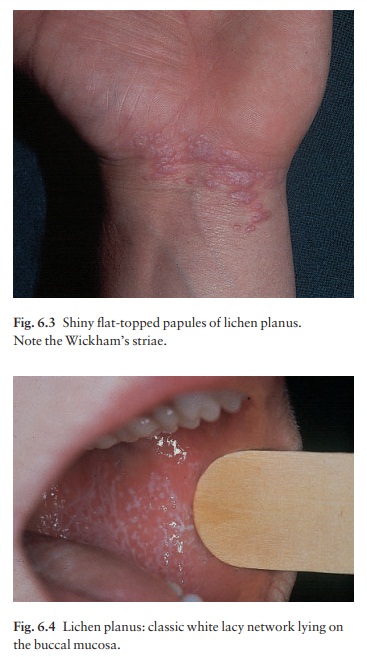
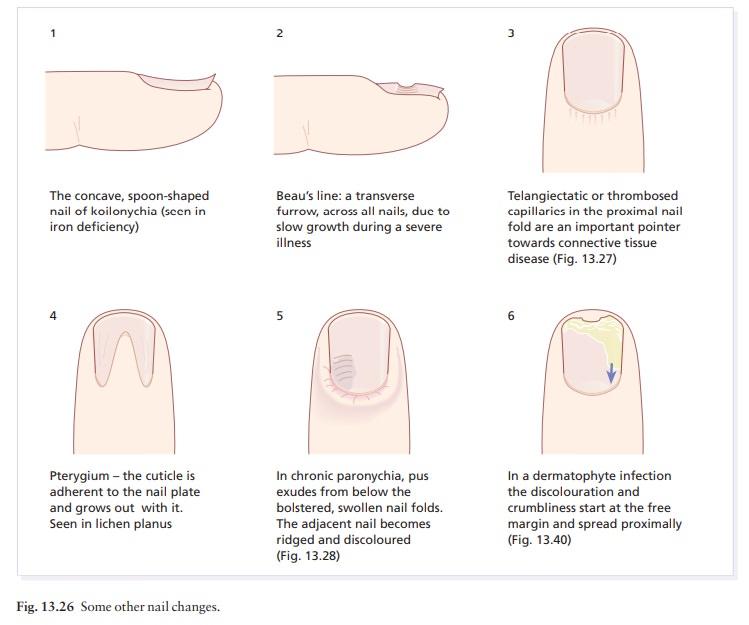
The genital skin may be similarly affected (see Fig. 13.37). Variants of the classical pattern are rare and often difficult to diagnose (Table 6.2). Curiously, although the skin plaques are usually itchy, patients rub rather than scratch, so that excoriations are uncommon. As in psoriasis, the Köbner phenomenon may occur (Fig. 6.5). The nails are usually normal, but in about 10% of patients show changes ranging from fine longitudinal grooves to destruction of the entire nail fold and bed (see Fig. 13.26). Scalp lesions can cause a patchy scarring alopecia.

Course
Individual
lesions may last for many months and the eruption as a whole tends to last
about 1 year. How-ever, the hypertrophic variant of the disease, with thick
warty lesions usually around the ankles (Fig. 6.6), often lasts for many years.
As lesions resolve, they become darker, flatter and leave discrete brown or
grey macules. About one in six patients will have a recurrence.

Complications
Nail
and hair loss can be permanent. The ulcerat-ive form of lichen planus in the
mouth may lead to squamous cell carcinoma. Ulceration, usually over bony
prominences, may be disabling, especially if it is on the soles. Any
association with liver disease is probably caused by the coexisting hepatitis
infections mentioned above.
Differential diagnosis
Lichen
planus should be differentiated from the other papulosquamous diseases listed
in Table 6.1. Lichenoid drug reactions can mimic lichen planus closely. Gold
and other heavy metals have often been implicated. Other drug causes include
antimalarials,
blockers, non-steroidal anti-inflammatory drugs, para-aminobenzoic acid, thiazide diuretics and penicillamine.
Contact with chemicals used to develop colour film can also produce similar
lesions. It may be hard to tell lichen planus from generalized dis-coid lupus
erythematosus if only a few large lesions are present, or if the eruption is on
the palms, soles or scalp. Wickham’s striae or oral lesions favour the
diagnosis of lichen planus. Oral candidiasis
can also cause confusion.
Investigations
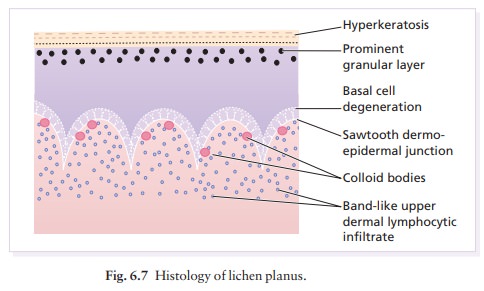
The
diagnosis is usually obvious clinically. The his-tology is characteristic (Fig.
6.7), so a biopsy will confirm the diagnosis if necessary.
Treatment
Treatment
can be difficult. If drugs are suspected as the cause, they should be stopped
and unrelated ones sub-stituted. Potent topical steroids will sometimes relieve
symptoms and flatten the plaques. Systemic steroid courses work too, but are
recommended only in special situations (e.g. unusually extensive involvement,
nail destruction or painful and erosive oral lichen planus). Treatment with
photochemotherapy with psoralen and ultraviolet A (PUVA;) or with narrow-band
UVB may reduce pruritus and help to
clear up the skin lesions. Acitretin (Formulary 2) has also helped some
patients with stubborn lichen planus. Antihistamines may blunt the itch. Mucous
membrane lesions are usually asymptomatic and do not require treatment; if they
do, then applications of a corticosteroid or tacrolimus in a gel base may be
helpful.
Related Topics