Chapter: Essentials of Psychiatry: Anxiety Disorders: Panic Disorder With and Without Agoraphobia
Panic Disorder: Assessment, Treatment
Assessment
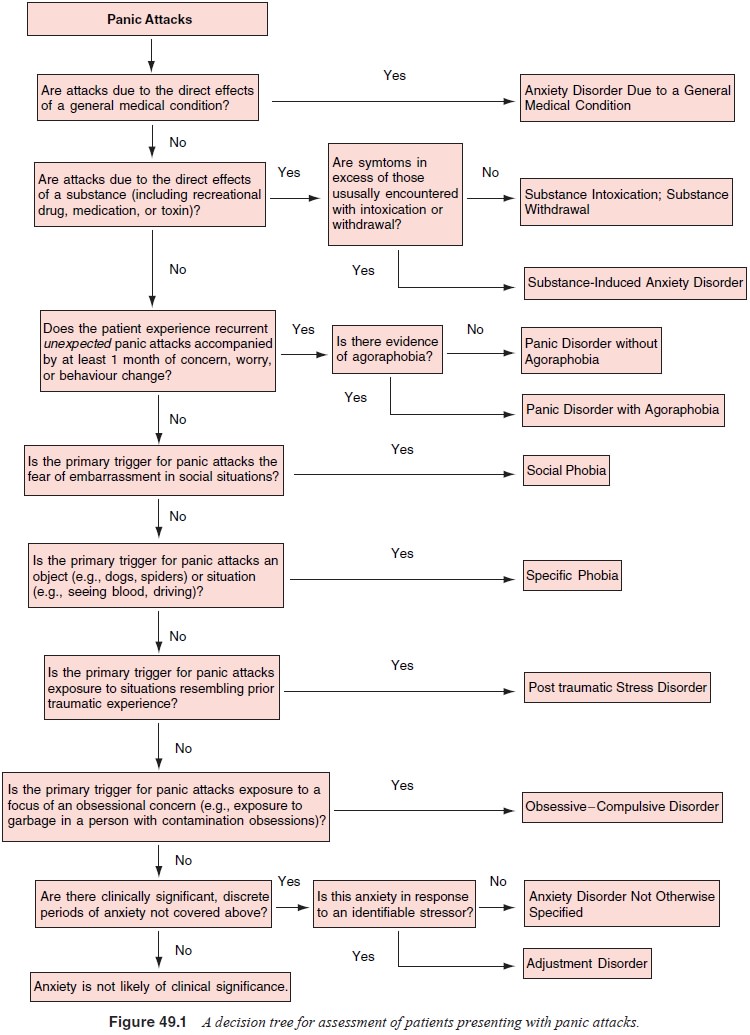
The most comprehensive and accurate diagnostic information emerges when
the clinician uses open ended questions and em-pathic listening, combined with
structured inquiry about specific events and symptoms. Useful structured
interviews include the Structured
Clinical Interview for DSM-IV (SCID-IV) and the Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV). A complete assessment for panic
disorder also includes a gen-eral medical evaluation consisting of a medical
history, review of organ systems, physical examination and blood tests. A
general medical evaluation is important for identifying general medical
conditions that mimic or exacerbate panic attacks or panic-like symptoms (e.g.,
seizure disorders, cardiac conditions, pheochro-mocytoma). These disorders
should be investigated and treated before contemplating a course of panic
disorder treatment. It is also important to rule out the other anxiety
disorders and major depressive disorder as primary factors in the person’s
panic at-tacks and avoidance prior to initiating treatment for panic disor-der
(Figure 49.1).
Diagnostic information can be usefully supplemented by short self-report
questionnaires to assess the severity of symp-toms and other variables. The Beck Depression Inventory and Beck Anxiety Inventory (Beck and Steer,
1987, 1993) are quick, reliable and
valid measures that can be administered at the start of each treatment session
to assess the severity of past-week general anxiety and depression. The Anxiety Sensitivity Index (Peterson and
Reiss, 1992) is another useful short questionnaire that can be used to gauge
the severity of the patient’s fear of bod-ily sensations. Scores on this scale
can be used to assess whether treatment is altering the patient’s tendency
catastrophically to misinterpret bodily sensations. This scale has good
reliabil-ity and validity, is sensitive to treatment-related effects, and its
post treatment scores predict who is likely to relapse after panic treatment.
Another
useful questionnaire to monitor treatment progress is the Panic and Agoraphobia Scale
(Bandelow, 1995). This 13-item scale was designed as a short, sensitive measure
for treatment outcome studies. The patient is asked to rate the past-week
frequency and/or severity of the following: 1) panic attacks, 2) agoraphobia, 3) anticipatory anxiety (i.e., worry about having an panic
attack), 4) panic-related disability in various areas of functioning, and 5)
worry about the health-related implications of panic (e.g., worry that panic
attacks will lead to a heart attack). The Panic and Agoraphobia Scale has good
reliability and valid-ity and is sensitive in detecting treatment-related
change. It has the advantage of providing a broad assessment of many features
of panic disorder and agoraphobia. A limitation is that it does not distinguish
between full and limited symptom panic attacks or among the types of panics
(i.e., unexpected, situationally bound, situationally predisposed). When asked
to recall their attacks, pa-tients may have difficulty making these distinctions.
Prospective (ongoing) monitoring is needed to provide this information.
To gain more detailed information on panic attacks, cli-nicians and
clinical researchers are increasingly including some form of prospective
monitoring in their assessment batteries. The most widely used are the panic attack records. The patient is
provided with a definition of a panic attack and then given a pad of panic
attack records that can be readily carried in a purse or pocket. The patient is
instructed to carry the records at all times and to complete one record (sheet)
for each full-blown or lim-ited symptom attack, soon after the attack occurs.
Variants on the panic diaries developed by Barlow and colleagues (Barlow and
Craske, 1994) are among the most informative and easy to use. These records are
then reviewed during treatment sessions to glean information about the links
among beliefs, bodily sensa-tions and safety behaviors, and to assess treatment
progress.
Treatment
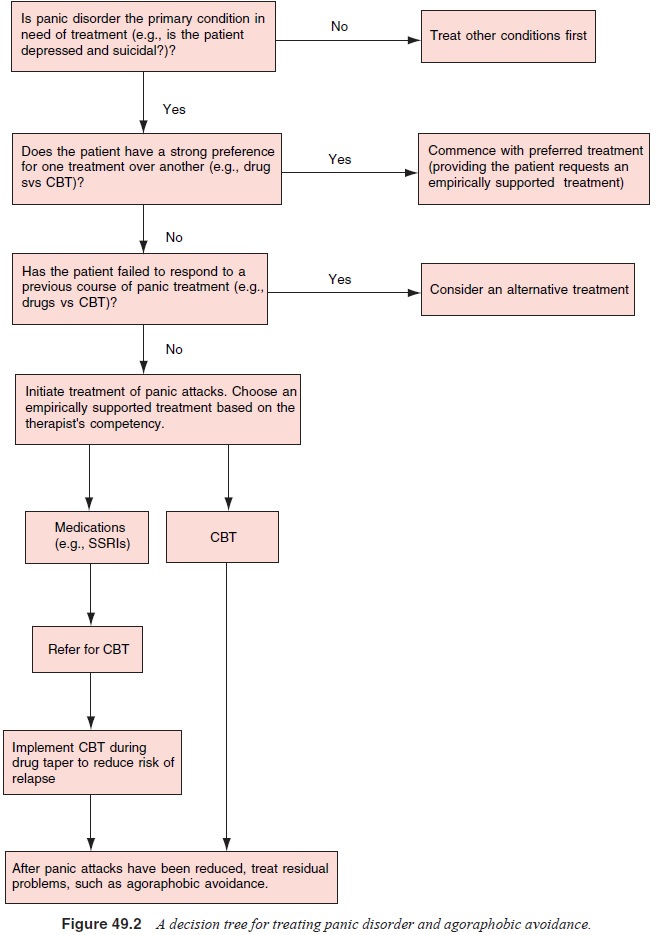
There are a number of approaches that can be taken in treating panic
disorder with and without agoraphobia. Both single and combined treatment
modalities are presented in Figure 49.2.
Related Topics