Chapter: Paediatrics: Gastroenterology and nutrition
Paediatrics: Parenteral nutrition
Parenteral nutrition
IV parenteral nutrition may be
supplemental or provide TPN. Parents can be trained to give prolonged PN at
home to children.
Indications
ŌĆó
Post-operative,
e.g. abdominal or cardiothoracic.
ŌĆó
Treatment
of IBD.
ŌĆó
After
severe trauma or burns.
ŌĆó
Acute
pancreatitis.
ŌĆó
Oral
feeds are contraindicated, e.g. NEC.
ŌĆó
Intestinal
failure, e.g. short bowel syndrome, congential enteropathy.
ŌĆó
Protracted
vomiting or diarrhoea.
ŌĆó
GI
obstruction, e.g. chronic intestinal pseudo-obstruction.
ŌĆó
Very
preterm infants.
ŌĆó
Oncology
patients, e.g. severe mucositis, graft versus host disease.
Administration
ŌĆó
A
multidisciplinary team of clinician, pharmacist, and paediatric dietitian
should be involved in supervising PN.
ŌĆó
Follow
unit/hospital dietetic/pharmacy guidelines for individual needs.
ŌĆó
Allowance
should be made of body weight (you may need to estimate a working weight, e.g.
if oedematous or gross ascites), recent weight trends, clinical condition,
fluid and nutritional requirements, additional infused fluids.
Method
Once requirements are calculated,
sterile pharmacy-prepared solutions are given via central (preferable) or
peripheral venous lines. Rapid com-mencement of PN may risk ŌĆśrefeeding
syndromeŌĆÖ in chronically under-nourished patients. When significant
malnutrition exists, measure and correct electrolyte abnormalities before
commencing PN and introduce slowly.
PN is usually supplied and
administered as two components.
ŌĆó
Lipid component: contains fat (triglyceride
emulsion, e.g. Intralipid 20%) and fat soluble vitamins. Usually
infused over 20hr.
ŌĆó
Aqueous component: contains carbohydrate (glucose
solution), protein (crystalline
L-amino acid solution), electrolytes, water soluble vitamins, minerals, trace
elements (zinc, copper, manganese, selenium, +/ŌĆō iron). Usually infused over
24hr.
Monitoring
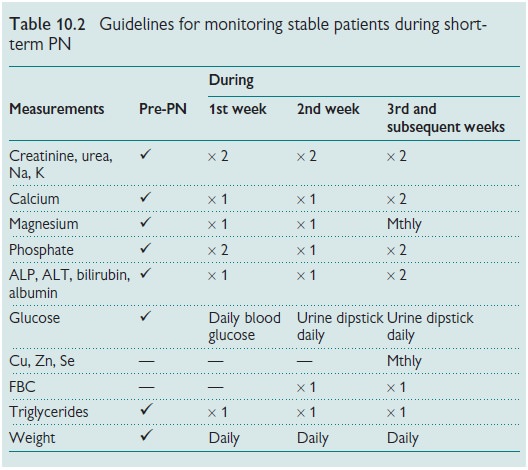
Serious, unexpected biochemical
disturbances occur rarely as a result of PN. An appropriate monitoring regimen
is suggested in Table 10.2.
Weaning
PN should be weaned slowly so that
hypoglycaemia is avoided. This also allows GI mucosal recovery as enteral
feeding is increased. When wean-ing is protracted parenteral nutrition can be
administered over shortened periods. A paediatric dietitian should assess the
contribution of both enteral and parenteral feeds to ensure nutritional
adequacy.
Complications/problems
ŌĆó
Sepsis: usually S. epidermidis, S.
aureus, Candida, Pseudomonas, E. coli.
ŌĆó
Demanding: in expertise, cost, etc.
ŌĆó
Central-line: occlusion, breakage, displacement.
ŌĆó
Electrolyte/metabolic disturbances: e.g. glucose ŌĆśriseŌĆÖor d.
ŌĆó
Vascular: thrombophlebitis,
thromboembolism, extravasation injuries.
ŌĆó
Cardiac tamponade: avoid by placing IV line tip
proximal to right atrium.
ŌĆó
From amino acids: PN-associated liver disease,
including, steatosis, cholestasis,
or, rarely cirrhosis or portal hypertension.
ŌĆó
From lipids: platelet dysfunction,
hyperlipidaemia, fatty liver, pulmonary hypertension.
ŌĆó Metabolic bone disease: due to insufficient Ca2+ and PO43 ŌĆō.
Related Topics